Practice Essentials
Multiple sclerosis (MS) is an immune-mediated inflammatory disease that attacks myelinated axons in the central nervous system, destroying the myelin and the axon in variable degrees and producing significant physical disability within 20–25 years in more than 30% of patients. White matter tracts are affected, including those of the cerebral hemispheres, infratentorium, and spinal cord. MS lesions, known as plaques, may form in CNS white matter in any location; thus, clinical presentations may be diverse. Continuing lesion formation in MS often leads to physical disability and, sometimes, to cognitive decline. [1] Magnetic resonance imaging (MRI) of the brain is useful in the diagnosis and treatment of multiple sclerosis.
Preferred examination
Radiologically, MRI has revolutionized the investigation, diagnosis, and even the treatment of MS. Usually, MRI is the only imaging modality needed for imaging patients with MS, and it far surpasses all other tests with respect to its positive predictive value. [1, 2, 3]
(See the images below.)
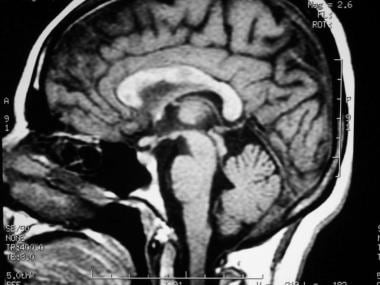 Sagittal T1-weighted MRI depicts multiple hypointense lesions in the corpus callosum; this finding is characteristic of multiple sclerosis.
Sagittal T1-weighted MRI depicts multiple hypointense lesions in the corpus callosum; this finding is characteristic of multiple sclerosis.
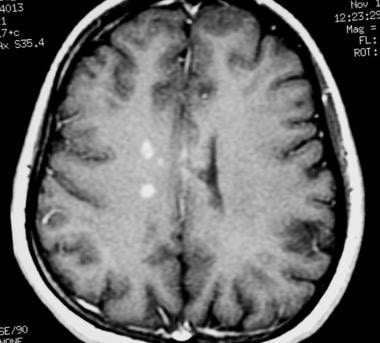
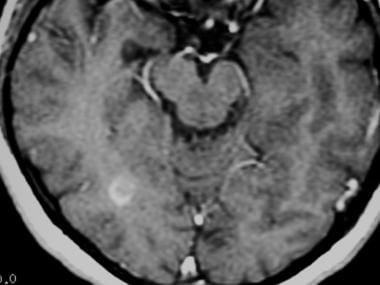
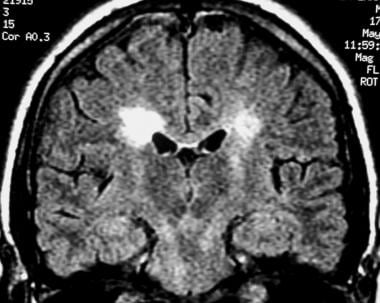 Coronal fluid-attenuated inversion recovery (FLAIR) MRI in a patient with multiple sclerosis demonstrates periventricular high–signal intensity lesions, which exhibit a typical distribution for multiple sclerosis. FLAIR MRI is a highly sensitive sequence for lesion detection, particularly supratentorially.
Coronal fluid-attenuated inversion recovery (FLAIR) MRI in a patient with multiple sclerosis demonstrates periventricular high–signal intensity lesions, which exhibit a typical distribution for multiple sclerosis. FLAIR MRI is a highly sensitive sequence for lesion detection, particularly supratentorially.
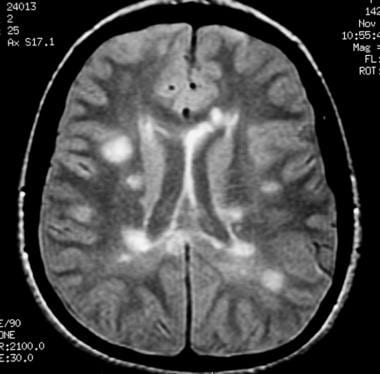
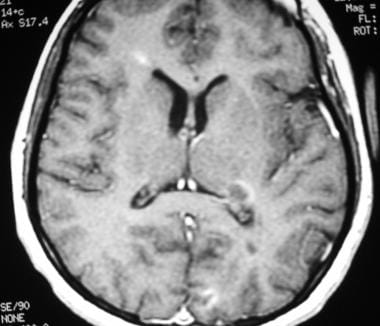
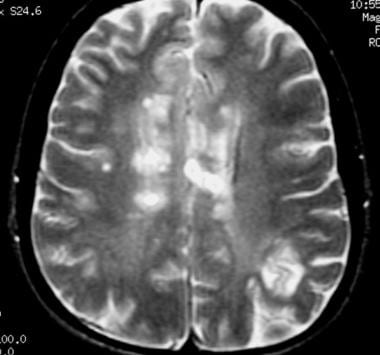 Axial T2-weighted MRI in a patient with multiple sclerosis demonstrates numerous white matter plaques in a callosal and pericallosal white matter distribution.
Axial T2-weighted MRI in a patient with multiple sclerosis demonstrates numerous white matter plaques in a callosal and pericallosal white matter distribution.
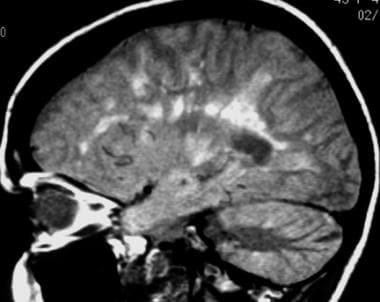
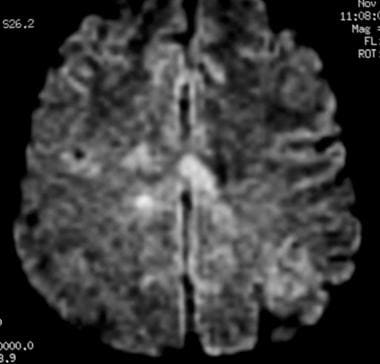 Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
One of the limitations of using MRI in patients with MS is the discordance occurring between lesion location and the clinical presentation. In addition, depending on the number and location of findings, MRI can vary greatly in terms of sensitivity and specificity in the diagnosis of MS.
Computed Tomography
Similar to radiography, computed tomography (CT) scanning has had a limited role in the diagnosis of MS and in the treatment of patients since the advent of MRI. CT scans may be used to exclude other causes of neurologic impairment, but they have a low positive predictive value in the diagnosis of MS; thus, the false-negative rate is high.
Prior to the use of MRI, CT scanning, with the injection of double or triple doses of intravenous contrast material, was used in attempts to identify active MS lesions. However, the scans were insensitive for the detection of chronic lesions. CT scans can help assess the degree of cerebral atrophy associated with advanced MS, but given the plethora of additional information provided by MRI, CT is no longer used for this purpose.
An acute MS lesion may enhance and appear simply as an enhancing white matter lesion on CT scans, but the appearance is highly nonspecific. When a highly active MS lesion is observed to enhance and possibly exerts mass effect, it can be termed tumefactive (due to the potential for misidentification as a tumor). Because CT scans typically do not help to identify the more chronic lesions, the tumefactive MS lesion may appear as a solitary enhancing mass, which leads to neurosurgical intervention. Fortunately, this situation is relatively uncommon.
In a cohort of 200 patients, Paty et al found that of the 19 who went on to develop clinically definite MS (CDMS), abnormal CT findings were demonstrated in only 9 (47%). In contrast, abnormal MRI findings were demonstrated in 18 (95%). All of the abnormal CT findings were also demonstrated on MRIs. [4]
Magnetic Resonance Imaging
The advent of MRI has revolutionized the diagnosis and monitoring of MS. MRI is well established as the preferred imaging modality for depicting MS lesions. In patients with clinically definite MS (CDMS), MRI demonstrates a high rate of abnormal findings compatible with the diagnosis. In a study by Lukes et al, lesions were demonstrated in 10 patients with CDMS. [23] In a larger study by Robertson et al, MRI findings were abnormal in 124 of 133 patients with CDMS. Ormerod et al found that 112 of 114 patients with CDMS had abnormal MRI findings and that 102 of 114 had discrete white matter lesions. [24]
Another major use of MRI has been the evaluation of patients who have had only 1 episode of neurologic impairment and who do not meet the clinical criteria for the diagnosis. The overall risk of developing MS after a single episode of neurologic impairment is estimated to be as low as 12% (2-yr follow-up study by Beck et al) to as high as 45% (12.9-yr follow-up study by Sandberg-Wollheim et al [25] ) or 58% (14.9-yr follow-up study by Rizzo et al [26] ).
MRI has been proven to be the most useful investigation for predicting the progression to MS. In a 10-year follow-up study of patients with a clinically isolated event, 45 (83%) of 54 patients with abnormal MRI findings went on to develop clinical MS, whereas only 3 of 27 with normal MRI findings developed MS. [27]
Tintoré et al followed up 70 patients for an average of 28.3 months after an isolated neurologic event and compared various MRI criteria for the diagnosis MS, as defined by Paty et al, Fazekas et al, and Barkhof et al. [4, 5, 28, 29] With the method of Paty et al, which requires 3 or 4 lesions (1 of which is periventricular), the authors reported a sensitivity of 86% but a specificity of only 54%. The criteria of Fazekas et al resulted in the same sensitivity and specificity. These criteria require 3 lesions with 2 of the 3 following characteristics: infratentorial location, periventricular location, and lesion greater than 6 mm. The criteria of Barkhof require 1 infratentorial lesion, 1 juxtacortical lesion, 3 periventricular lesions, and either 1 gadolinium-enhanced lesion or more than 9 lesions on T2-weighted MRI scans. These criteria resulted in a sensitivity of 73% and a specificity of 73%. Thus, as the MRI criteria become more stringent in the diagnosis of MS, specificity increases at the expense of decreasing sensitivity.
In a cohort of the BENEFIT study (a multicenter, randomized, clinical study of 468 patients), the modified Barkhof criteria showed moderate predictive value for conversion to CDMS over 3 years, despite the fact that all patients received interferon beta-1b therapy for at least 1 year. Follow-up MRI was found to be most informative after 9 months in patients without dissemination in space at baseline. The overall conversion rate to CDMS was 42%. Barkhof criteria with the strongest prognostic value were the presence at baseline of at least 9 T2-weighted lesions and at least 3 periventricular lesions. [30]
According to a study of postmortem MS tissue by Pitt et al, 3-dimensional (3-D), T2*-weighted, gradient-echo (T2*GRE) and white matter–attenuated, turbo-field-echo (TFE) sequences at a 7T field strength can detect most cortical lesions. The 3-D T2*GRE and white matter–attenuated TFE sequences retrospectively detected 93% and 82% of all cortical lesions, respectively. [31]
Susceptibility MRI contrast variations reflect alterations in brain iron and myelin content. In 24 MS patients (306 white matter lesions) who underwent 7T MRI of the brain, most lesions were hypointense on R2*. Hyperintense lesions on quantitative susceptibility mapping were more frequent in relapsing-remitting MS than in progressive MS. Hyperintense lesion rims on quantitative susceptibility maps were more common in progressive MS and in patients with higher levels of disability and fatigue. Mean lesion R2* was inversely related to disability and fatigue and significantly reduced in progressive MS. Relative susceptibility was lower in lesions in progressive MS than in relapsing-remitting MS. [32]
Typical findings and pulse sequences
Because of the inflammation and breakdown of the blood-brain barrier in MS lesions, the presence of extravascular fluid leads to hyperintensity on T2-weighted images. Thus, in a patient with MS, MRI scans typically demonstrate more than 1 hyperintense white matter lesion. [33, 34, 35, 36, 37]
Lesions may be observed anywhere in the CNS white matter, including the supratentorium, infratentorium, and spinal cord; however, more typical locations for MS lesions include the periventricular white matter, brainstem, cerebellum, and spinal cord. Ovoid lesions perpendicular to the ventricles are common in MS and occasionally are called Dawson bars or fingers, which occur along the path of the deep medullary veins. Perhaps the most specific lesions in MS are noted in the corpus callosum at the interface with the septum pellucidum. [38]
(See the MRI scans below.)
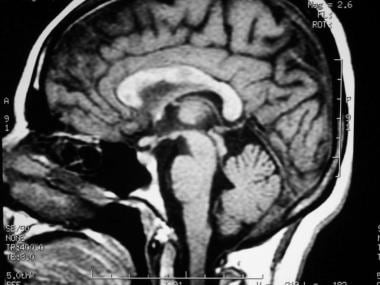 Sagittal T1-weighted MRI depicts multiple hypointense lesions in the corpus callosum; this finding is characteristic of multiple sclerosis.
Sagittal T1-weighted MRI depicts multiple hypointense lesions in the corpus callosum; this finding is characteristic of multiple sclerosis.
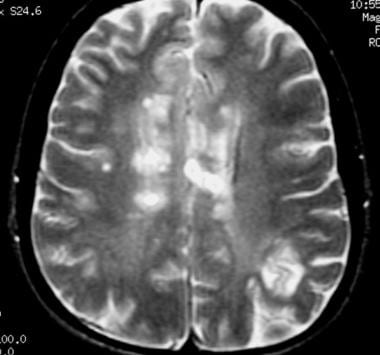 Axial T2-weighted MRI in a patient with multiple sclerosis demonstrates numerous white matter plaques in a callosal and pericallosal white matter distribution.
Axial T2-weighted MRI in a patient with multiple sclerosis demonstrates numerous white matter plaques in a callosal and pericallosal white matter distribution.
 Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis demonstrates several intensely enhancing pericallosal white matter lesions compatible with active disease.
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis demonstrates several intensely enhancing pericallosal white matter lesions compatible with active disease.
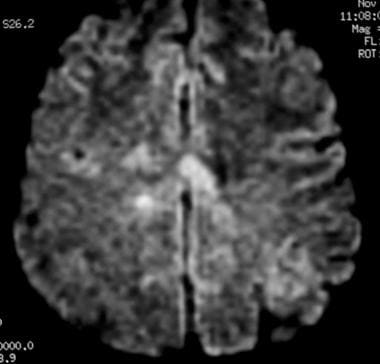 Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
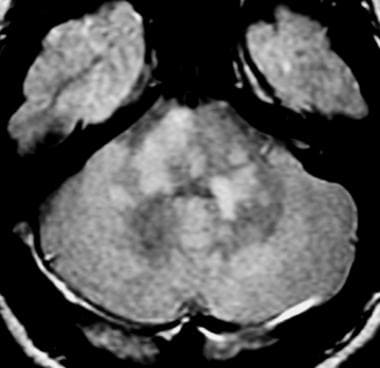 Axial proton density–weighted MRI through the posterior fossa in a patient with multiple sclerosis demonstrates multiple bright foci in the brainstem and cerebellum. Proton density–weighted sequences are highly sensitive for the detection of plaques in multiple sclerosis, especially in the posterior fossa.
Axial proton density–weighted MRI through the posterior fossa in a patient with multiple sclerosis demonstrates multiple bright foci in the brainstem and cerebellum. Proton density–weighted sequences are highly sensitive for the detection of plaques in multiple sclerosis, especially in the posterior fossa.
 Axial proton density–weighted MRI demonstrates multiple lesions in a distribution characteristic of multiple sclerosis. Specifically, the periventricular lesions and the more peripheral white matter lesions near the gray matter–white matter junction are typical MRI findings in multiple sclerosis.
Axial proton density–weighted MRI demonstrates multiple lesions in a distribution characteristic of multiple sclerosis. Specifically, the periventricular lesions and the more peripheral white matter lesions near the gray matter–white matter junction are typical MRI findings in multiple sclerosis.
 Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts enhancement of a plaque in the right temporo-occipital lobe, signifying disease activity. Note the C-shaped, or arclike, enhancement, which is fairly characteristic of multiple sclerosis.
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts enhancement of a plaque in the right temporo-occipital lobe, signifying disease activity. Note the C-shaped, or arclike, enhancement, which is fairly characteristic of multiple sclerosis.
 Sagittal proton density–weighted MRI in a patient with multiple sclerosis demonstrates the characteristic corpus callosal and pericallosal white matter lesions.
Sagittal proton density–weighted MRI in a patient with multiple sclerosis demonstrates the characteristic corpus callosal and pericallosal white matter lesions.
 Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts several enhancing lesions, at least 2 of which show characteristic C-shaped, or arclike, peripheral enhancement.
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts several enhancing lesions, at least 2 of which show characteristic C-shaped, or arclike, peripheral enhancement.
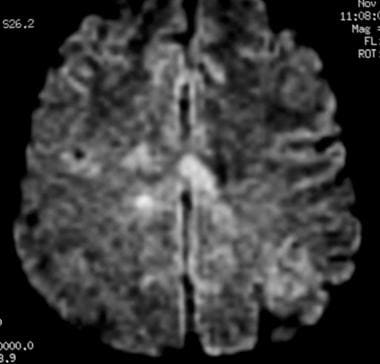 Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
Proton density (PD)–weighted MRI has an advantage over standard T2 imaging, because on PD series, MS lesions remain hyperintense, while the CSF signal is suppressed. Therefore, the lesions are easily identified. Depending on the PD technique, the CSF signal is suppressed to a variable degree, rendering it isointense to hypointense relative to the brain parenchyma. This sequence results in substantial suppression of Virchow-Robin spaces, which are perivascular CSF spaces that may penetrate to the subcortical white matter. These spaces may appear as hyperintense spots on standard T2-weighted MRI scans.
Compared with other techniques, nonenhanced T1-weighted MRI is far less sensitive in detecting MS lesions. Acute lesions usually are not depicted at all. With T1-weighted MRI, the clinician can gain a general appreciation of the global cerebral atrophy that occurs with advanced chronic MS. Global atrophy has been suggested to have the strongest imaging correlation with disability.
Chronic MS lesions usually result in localized leukomalacia, and they may appear as hypointense lesions that represent loss of tissue.
Gadolinium-enhanced T1-weighted MRI scans can depict acute, active MS lesions. These appear as enhancing white matter lesions; the presence of an enhancing lesion has been shown to increase the specificity for MS. [5, 28]
FLAIR MRI
Newer MRI pulse sequences and techniques, including fluid-attenuated inversion recovery (FLAIR) MRI and MR spectroscopy, have emerged that are potentially useful in the evaluation of patients with MS.
FLAIR MRI is a heavily T2-weighted technique that dampens the ventricular (ie, free-water) CSF signal. Thus, the highest signals on the sequence are from certain brain parenchymal abnormalities, such as MS lesions, while the CSF appears black. This appearance is different from that on PD-weighted MRIs, on which periventricular MS lesions may appear nearly isointense to the adjacent CSF.
MTR-based imaging or multi-compartment diffusion imaging might be useful to investigate the effect of drugs promoting remyelination, while post-contrast FLAIR could be applied to investigate the monitoring response to drugs targeting B cells. [39]
(See the image below.)
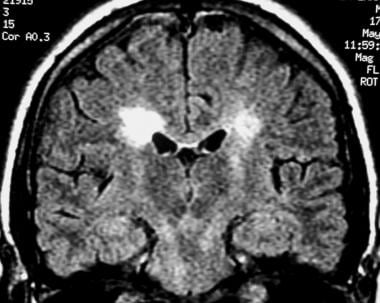 Coronal fluid-attenuated inversion recovery (FLAIR) MRI in a patient with multiple sclerosis demonstrates periventricular high–signal intensity lesions, which exhibit a typical distribution for multiple sclerosis. FLAIR MRI is a highly sensitive sequence for lesion detection, particularly supratentorially.
Coronal fluid-attenuated inversion recovery (FLAIR) MRI in a patient with multiple sclerosis demonstrates periventricular high–signal intensity lesions, which exhibit a typical distribution for multiple sclerosis. FLAIR MRI is a highly sensitive sequence for lesion detection, particularly supratentorially.
The greater relative suppression of CSF on FLAIR images compared with PD-weighted series increases the contrast between periventricular lesions and CSF, enhancing their detection. FLAIR has been shown to be superior to PD-weighted sequences in the detection of MS lesions in the cerebral hemispheres. However, PD-weighted imaging remains the investigation of choice for infratentorial lesions. [40]
MR spectroscopy
Magnetic resonance (MR) spectroscopy uses the characteristic spectra of specific biochemical markers to quantitate organic compounds in vivo. N -acetylaspartate (NAA) is a relatively specific neuronal marker that is present in sufficient concentrations in the brain to be revealed on MR spectroscopic images. By comparing the spectral signal of NAA with that of creatinine (Cr), MR spectroscopy can be useful in assessing neuronal and axonal loss.
Arnold et al noted that the NAA-Cr ratio in the CNS was decreased in moderate to advanced MS. White matter that appeared normal on T1- and T2-weighted images also demonstrated the reduction. [41] In addition, a normal ratio was noted in the area of a recently active lesion associated with clinical deficits that subsequently resolved. The findings led the authors to propose that MR spectroscopic findings may be able to help identify irreversible axonal damage.
In a study involving 88 patients with MS, De Stefano et al found a strong correlation between disability scores and NAA-Cr ratios. [42] The ratio exhibited a stronger correlation in patients with MS patients who had milder disability scores. Because MR spectroscopy appears to be capable of depicting changes in white matter that are not detected with routine pulse sequences and because the findings are correlated with disability scores, the use of MR spectroscopy may prove valuable in monitoring patients after treatment and in formulating their prognosis.
Nonstandard MRI sequences
Beyond the standard MRI sequences that are used in clinical practice (T1 +/- Gad, T2, diffusion-weighted imaging, FLAIR), more advanced MRI techniques have been used for research purposes. Many of these series require greater magnetic field strengths over the popular 1.5T, but with the increasing availability of 3T MRI, these sequences will likely find their way more and more into standard clinical practice. [43]
Diffusion tensor imaging (DTI) can utilize diffusion-weighted imaging techniques in different orientations to establish pathology along white matter tracts in the CNS. DTI can identify demyelination and loss of axons along tracts that would otherwise go undetected by conventional techniques. [44, 45, 46] DTI can also identify disease activity in and injury to gray matter structures, which in turn can be used as markers of disease activity and severity. [47, 48, 49, 50]
Double inversion recover (DIR) sequences can also detect cortical lesions with increased sensitivity over standard MRI sequences, with higher MRI field strengths improving sensitivity. [51, 52]
Magnetization transfer imaging (MTI) is capable of identifying MS lesions before they can be detected by conventional MRI techniques. [53, 54] Magnetization transfer ratio (MTR)—based imaging or multi-compartment diffusion imaging might be useful to investigate the effect of drugs promoting remyelination, while post-contrast FLAIR could be applied to investigate the monitoring response to drugs targeting B cells.
Limitations
In virtually all patients with clinically well-established MS, MRI scans demonstrate the corresponding changes. False-negative findings occur more frequently in patients with early MS and a minimal clinical history of neurologic impairment than in other patients.
O'Riordan et al prospectively found that in 3 of 27 patients with normal MRI findings, MS subsequently developed. [27] However, the patients with normal MRI findings all developed lesions detectable on MRI scans when the disease became established. Similarly, as patients are followed for longer periods, the rate of false-positive findings decreases, because in many patients with abnormal MRI findings after a single neurologic event, the clinical criteria for MS eventually develop.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF), also called nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MR angiography scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
Ultrasonography is not currently used in the investigation of MS. Berg et al, however, used transcranial sonography to determine the size of the ventricles in patients with MS and found that an increasing size is correlated with the MRI-determined brain volume, as well as with cognitive dysfunction and clinical disability. Further studies may establish a role for ultrasonography in the prognosis and treatment of patients with MS. [55]
According to Walter et al, in patients with MS, hyperechogenicity of the substantia nigra and lenticular nucleus correlates with more pronounced MRI T2 hypointensity, which is thought to reflect iron deposition, and a larger bilateral substantia nigra echogenic area is related to a higher rate of disease progression. In addition, a small echogenic area predicts a disease course without further progression over 2 years. [56] Walter et al performed the study to determine whether transcranial ultrasonography can identify lesions in deep gray matter in patients with MS and whether such findings can identify the severity and progression of MS. Of 75 patients followed, abnormal hyperechogenicity of the substantia nigra occurred in 41%; of the lenticular nucleus, in 54%; of the caudate nucleus, in 40%; and of the thalamus, in 8%, with similar frequency in patients with relapsing-remitting and primary or secondary progressive MS if corrected for disease duration.
Tromba et al used Italian researcher Paolo Zamboni’s ultrasound protocol, along with M-mode ultrasound, and found that about 60% of 112 patients with MS had venous insufficiency, [57] but in a Canadian study using catheter venography, Traboulsee et al found that only 1 of 65 patients (2%) with MS had extracranial venous narrowing. [58] The Canadian study also utilized the ultrasound criteria proposed by Zamboni and found that 35 of 79 (44%) MS patients met the criteria for cerebrospinal venous insufficiency. The Canadian researchers concluded that the ultrasound criteria are neither sensitive nor specific for narrowing on catheter venography. [58]
Macgowan et al looked at venous cerebral outflow in 26 MS patients and 26 controls using ultrasound and found no difference between the 2 groups. They also used phase-contrast MRI and found no significant difference in venous flow in the vertebral arteries, internal jugular veins, and epidural veins. [59]
-
Sagittal T1-weighted MRI depicts multiple hypointense lesions in the corpus callosum; this finding is characteristic of multiple sclerosis.
-
Axial T2-weighted MRI in a patient with multiple sclerosis demonstrates numerous white matter plaques in a callosal and pericallosal white matter distribution.
-
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis demonstrates several intensely enhancing pericallosal white matter lesions compatible with active disease.
-
Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.
-
Axial proton density–weighted MRI through the posterior fossa in a patient with multiple sclerosis demonstrates multiple bright foci in the brainstem and cerebellum. Proton density–weighted sequences are highly sensitive for the detection of plaques in multiple sclerosis, especially in the posterior fossa.
-
Coronal fluid-attenuated inversion recovery (FLAIR) MRI in a patient with multiple sclerosis demonstrates periventricular high–signal intensity lesions, which exhibit a typical distribution for multiple sclerosis. FLAIR MRI is a highly sensitive sequence for lesion detection, particularly supratentorially.
-
Axial proton density–weighted MRI demonstrates multiple lesions in a distribution characteristic of multiple sclerosis. Specifically, the periventricular lesions and the more peripheral white matter lesions near the gray matter–white matter junction are typical MRI findings in multiple sclerosis.
-
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts enhancement of a plaque in the right temporo-occipital lobe, signifying disease activity. Note the C-shaped, or arclike, enhancement, which is fairly characteristic of multiple sclerosis.
-
Point-resolved spectroscopic study performed in a patient with multiple sclerosis demonstrates a slightly decreased N-acetylaspartate peak and a mildly elevated choline peak; these findings are compatible with demyelination with neuronal loss and increased cell membrane turnover.
-
Sagittal proton density–weighted MRI in a patient with multiple sclerosis demonstrates the characteristic corpus callosal and pericallosal white matter lesions.
-
Axial T1-weighted, gadolinium-enhanced MRI in a patient with multiple sclerosis depicts several enhancing lesions, at least 2 of which show characteristic C-shaped, or arclike, peripheral enhancement.
-
Axial diffusion-weighted MRI in a patient with multiple sclerosis shows several hyperintense lesions, a feature of inflammatory disease activity.

