Practice Essentials
Pancoast tumors are neoplasms of pulmonary origin located at the apical pleuropulmonary groove (superior sulcus). [1, 2] By direct extension, Pancoast tumors typically involve the lower trunks of the brachial plexus, intercostal nerves, stellate ganglion, adjacent ribs, and vertebrae. As a result, patients may present with severe pain, often of neuropathic characteristics radiating toward the ipsilateral upper extremity and accompanied with sympathetic symptoms (eg, the Horner syndrome) caused by invasion of the cervicothoracic sympathetic ganglion. These manifestations may appear months before the diagnosis of the underlining disease. [3, 4, 5, 6]
Pancoast syndrome is characterized by ipsilateral shoulder and arm pain, paresthesias, paresis and atrophy of the thenar muscles of the hand, and Horner syndrome (ptosis, miosis, and anhidrosis). [7]
More than 95% of Pancoast tumors are non–small cell carcinomas, most commonly squamous cell carcinomas (52%) or adenocarcinomas and large cell carcinomas (approximately 23% for each subtype). [1] Small cell carcinomas are seen in fewer than 5% of cases. [8]
Staging of Pancoast tumor involves the tumor, node, and metastasis (TNM) classification system, in which T indicates site and size of the primary tumor, N is related to nodal involvement according to site, and M indicates the presence or absence of distant metastases. These tumors are, at a minimum, T3N0M0 (T3 for chest wall invasion, stage IIB), and they are considered T4 lesions if the brachial plexus, mediastinal structures, or vertebral bodies are involved at the time of presentation.
Radiography
Posteroanterior (PA) chest radiographs may show unilateral apical opacity (as seen in the first image below), pleural thickening, asymmetry of the apices greater than 5 mm (see the second image below), or a large mass, depending on the tumor stage during diagnosis. Although it is less accurate than CT, chest radiography can show a peripheral lesion and its size. Local rib destruction and/or tracheal deviation can sometimes be observed. Mediastinal enlargement can be seen as well. Lordotic chest views can be beneficial, but the findings can also be misleading. In the early stages, Pancoast tumors are difficult to detect on PA chest radiographs because of the difficulty in interpreting overlying shadows at the apices. [19]
(See the images below.)
 A 74-year-old male with Pancoast tumor. A chest radiograph shows a right apical soft-tissue speculated mass. Erosion of the adjacent ribs is not evident; hence, the value of CT scan (seen in CT section of this article).
A 74-year-old male with Pancoast tumor. A chest radiograph shows a right apical soft-tissue speculated mass. Erosion of the adjacent ribs is not evident; hence, the value of CT scan (seen in CT section of this article).
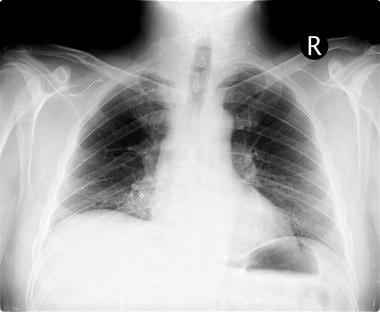 Pancoast tumor. A 53-year-old man with a 50 pack-year history of smoking began experiencing upper back pain for several weeks. PA chest radiograph shows asymmetry of the apices (superior sulcus). The right apex is more opaque than the left. When the image is enlarged, the partially destroyed second and third right posterior ribs near the costovertebral junction can be seen.
Pancoast tumor. A 53-year-old man with a 50 pack-year history of smoking began experiencing upper back pain for several weeks. PA chest radiograph shows asymmetry of the apices (superior sulcus). The right apex is more opaque than the left. When the image is enlarged, the partially destroyed second and third right posterior ribs near the costovertebral junction can be seen.
Computed Tomography
CT and MRI are the most accurate imaging modalities in the identification and staging of Pancoast tumors, but CT is more economical and available. For T staging, CT is the most common modality and can help identify proximity to surrounding blood vessels, infiltration of the esophagus and trachea, and mediastinal invasion. Although CT can aid in detecting chest wall invasion, MRI has greater specificity and sensitivity in doing so. [20]
CT scanning is the best imaging modality for demonstrating bony destruction (see the first image below). In a study of 31 patients with superior pulmonary sulcus tumors, [10] CT scanning had a sensitivity of 60% and a specificity of 65%, with an overall accuracy of 63% in identification of extent of disease. Furthermore, contrast-enhanced CT has a reported sensitivity of 68-85% in detecting liver metastases. [21]
(See the images below.)
 Pancoast tumor. Axial nonenhanced CT image of the upper dorsal spine demonstrates a soft-tissue mass destroying the vertebra on the right and the right posterior elements, including the pedicle and part of the posterior spinous process.
Pancoast tumor. Axial nonenhanced CT image of the upper dorsal spine demonstrates a soft-tissue mass destroying the vertebra on the right and the right posterior elements, including the pedicle and part of the posterior spinous process.
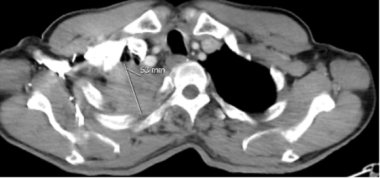 A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lung apices shows a soft-tissue mass lesion of 5.3 cm in the right apex.
A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lung apices shows a soft-tissue mass lesion of 5.3 cm in the right apex.
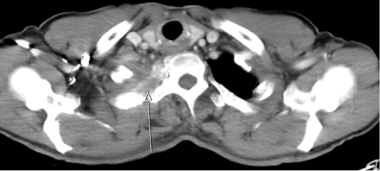 A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lungs apices at a different level shows erosion of the right second rib (arrow).
A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lungs apices at a different level shows erosion of the right second rib (arrow).
 A 50-year-old male with Pancoast tumor. An axial CT scan at the level of the apices demonstrates a soft-tissue mass with central necrosis and microcalcifications.
A 50-year-old male with Pancoast tumor. An axial CT scan at the level of the apices demonstrates a soft-tissue mass with central necrosis and microcalcifications.
Magnetic Resonance Imaging
MRI provides superior delineation of the normal anatomy of the brachial plexus because of its multiplanar capabilities. Advantages of MRI include the identification of the absence of streak artifact from bone and the accurate identification of blood vessels. It also provides superior soft-tissue contrast enhancement, and it is more accurate than other methods in documenting or excluding brachial plexus involvement by tumor. [22]
In a study of 31 patients with Pancoast tumors, MRI had a sensitivity of 88%, a specificity of 100%, and an overall accuracy of 94%. [10]
Compared to other techniques, MRI is more accurate in the evaluation of extension of tumor to the vertebral body, spinal canal, brachial plexus, and subclavian artery. This ability is important because invasion of the vertebral body, spinal canal, or upper brachial plexus is a contraindication to surgical resection. Also CT scanning appears to be superior to MRI in detecting chest wall invasion. The anatomy above the lung apex is better demonstrated on multiplanar MRI because the nerves of the brachial plexus and blood vessels follow a horizontal and parallel course, meeting above the apex of the lung.
(See the images below.)
 Pancoast tumor. Sagittal fast spin-echo T2-weighted MRI shows collapsed vertebrae and cord compression at C7, T1, and T2 caused by a soft tissue mass.
Pancoast tumor. Sagittal fast spin-echo T2-weighted MRI shows collapsed vertebrae and cord compression at C7, T1, and T2 caused by a soft tissue mass.
 Pancoast tumor. Sagittal gradient-echo T2-weighted MRI demonstrates a soft-tissue mass involving C7, T1, and T2, with collapse of the vertebrae and moderate cord compression.
Pancoast tumor. Sagittal gradient-echo T2-weighted MRI demonstrates a soft-tissue mass involving C7, T1, and T2, with collapse of the vertebrae and moderate cord compression.
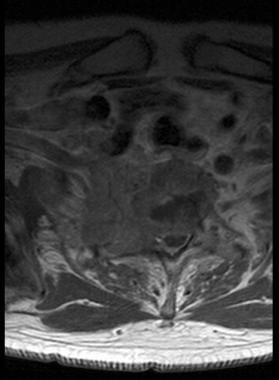 Pancoast tumor. Axial T1-weighted image shows cord compression caused by a large, enhancing mass. The right subclavian artery is not involved.
Pancoast tumor. Axial T1-weighted image shows cord compression caused by a large, enhancing mass. The right subclavian artery is not involved.
Ultrasonography
Some researchers have suggested that all patients with Pancoast tumors should undergo ultrasonographic examination of the ipsilateral scalene area and that percutaneous biopsy should be performed on nodes with a transverse diameter greater than 1 cm. The purpose of these studies is to assist in staging of the disease. The use of a sector ultrasonographic unit with a supraclavicular approach has been useful in guiding needle aspirations, with a yield for pathologic diagnosis in 91% of cases. [5, 14, 15]
Furthermore, ultrasonography can also be used to identify chest wall invasion. In one study, ultrasonography had a higher sensitivity (89%) than CT scanning (42%) and had a similar specificity in assessing chest wall invasion by lung tumors. [23]
Ultrasonography is also used in the detection of liver metastasis from lung tumors. [21]
Nuclear Imaging
Althought positron emission tomography (PET) is widely used in evaluating lung cancer patients, some research has revealed that it not suitable for all patients. The significance of PET greatly depends on clinical settings. For instance, PET is most useful in identifying patients with a high risk of metastasis (M1). It is also used in cases in which it is difficult to specify through other modalities whether a tumor is in N2 or N3 nodal involvement. [24]
PET is superior to CT imaging in detecting mediastinal and hilar node metastases. A meta-analyses compared detection of mediastinal nodal involvement by PET and CT imaging in patients with non–small cell lung cancer. The study showed that CT had a sensitivity and specificity of 60% and 77%, respectively, whereas PET had a sensitivity and specificity of 79% and 91%, respectively, concluding that PET is superior in mediastinal staging. [25] However, integrated PET-CT provides greater information in staging, with one study showing that PET-CT had greater diagnostic accuracy in staging of non–small cell lung cancer than either imaging modality used individually. [26]
(See the images below.)
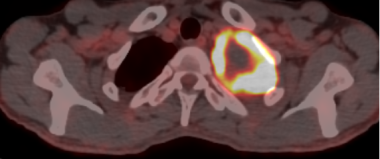
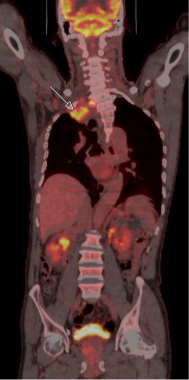 A 74-year-old male with Pancoast tumor. A PET scan shows an FDG-avid right-upper-lobe speculated mass inseparable from pleura and chest wall.
A 74-year-old male with Pancoast tumor. A PET scan shows an FDG-avid right-upper-lobe speculated mass inseparable from pleura and chest wall.
-
Pancoast tumor. A 53-year-old man with a 50 pack-year history of smoking began experiencing upper back pain for several weeks. PA chest radiograph shows asymmetry of the apices (superior sulcus). The right apex is more opaque than the left. When the image is enlarged, the partially destroyed second and third right posterior ribs near the costovertebral junction can be seen.
-
Pancoast tumor. Axial nonenhanced CT image of the upper dorsal spine demonstrates a soft-tissue mass destroying the vertebra on the right and the right posterior elements, including the pedicle and part of the posterior spinous process.
-
Pancoast tumor. Sagittal fast spin-echo T2-weighted MRI shows collapsed vertebrae and cord compression at C7, T1, and T2 caused by a soft tissue mass.
-
Pancoast tumor. Sagittal gradient-echo T2-weighted MRI demonstrates a soft-tissue mass involving C7, T1, and T2, with collapse of the vertebrae and moderate cord compression.
-
Pancoast tumor. Axial T1-weighted image shows cord compression caused by a large, enhancing mass. The right subclavian artery is not involved.
-
A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lung apices shows a soft-tissue mass lesion of 5.3 cm in the right apex.
-
A 74-year-old male with Pancoast tumor. A chest radiograph shows a right apical soft-tissue speculated mass. Erosion of the adjacent ribs is not evident; hence, the value of CT scan (seen in CT section of this article).
-
A 74-year-old male with Pancoast tumor. An axial CT scan at the level of the lungs apices at a different level shows erosion of the right second rib (arrow).
-
A 50-year-old male with Pancoast tumor. An axial CT scan at the level of the apices demonstrates a soft-tissue mass with central necrosis and microcalcifications.
-
A 50-year-old male with Pancoast tumor. A coronal reformat of the above CT scan shows further relations with the adjacent structures without definite evidence of invasion.
-
A 74-year-old male with Pancoast tumor. A PET scan shows an FDG-avid right-upper-lobe speculated mass inseparable from pleura and chest wall.
-
A 50-year-old man with Pancoast tumor. A PET scan shows an FDG-avid left-upper-lobe mass with no definite evidence of invasion of the adjacent structures. Histology reports non-small cell lung cancer.