Practice Essentials
The most common mass in the popliteal fossa, Baker cyst, also termed popliteal cyst, results from fluid distention of the gastrocnemio-semimembranosus bursa, which is located in the medial aspect of the popliteal fossa. [1] The eponym honors the work of Dr William Morrant Baker. In 1877, Baker described 8 cases of periarticular cysts caused by synovial fluid that had escaped from the knee joint and formed a new sac outside the joint. [2] The common underlying conditions were osteoarthritis and Charcot joint. [3, 4]
Baker cysts can be associated with conditions such as osteoarthritis of the knee, meniscal tears, rheumatoid arthritis, Charcot joints, and synovial disorders of the knee. The majority of patients with Baker cysts are asymptomatic, but knee joint pain and stiffness and a palpable mass in the medial popliteal fossa are not uncommon. The manifestations of a ruptured cyst can resemble those of deep venous thrombosis (DVT) or thrombophlebitis [5, 6, 7, 8, 9, 10]
(See the images below.)
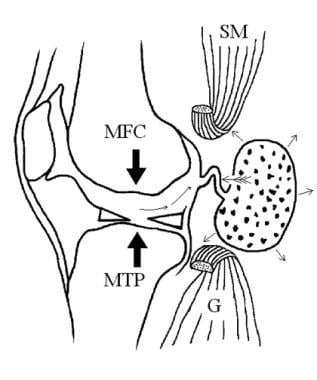 Valvular mechanism of Baker cyst. Effusion and fibrin are pumped (large arrows) into the Baker cyst (long, thin arrows). In the Bunsen-valve mechanism, the enlarging Baker cyst exerts mass effect (feathered arrow) on the slitlike communication between the joint and the cyst, trapping effusion. In the ball-valve mechanism, fibrin serves as a 1-way valve that prevents the effusion's return to the knee joint. Trapped effusion is reabsorbed through the semipermeable membrane (short, thin arrows), leaving behind concentrations of fibrin. (MFC: medial femoral condyle; MTP: medial tibial plateau; G: medial head of gastrocnemius muscle; SM: semimembranosus muscle)
Valvular mechanism of Baker cyst. Effusion and fibrin are pumped (large arrows) into the Baker cyst (long, thin arrows). In the Bunsen-valve mechanism, the enlarging Baker cyst exerts mass effect (feathered arrow) on the slitlike communication between the joint and the cyst, trapping effusion. In the ball-valve mechanism, fibrin serves as a 1-way valve that prevents the effusion's return to the knee joint. Trapped effusion is reabsorbed through the semipermeable membrane (short, thin arrows), leaving behind concentrations of fibrin. (MFC: medial femoral condyle; MTP: medial tibial plateau; G: medial head of gastrocnemius muscle; SM: semimembranosus muscle)
 Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
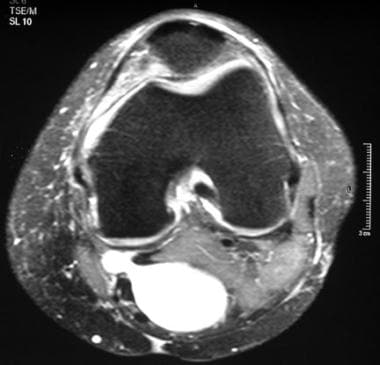
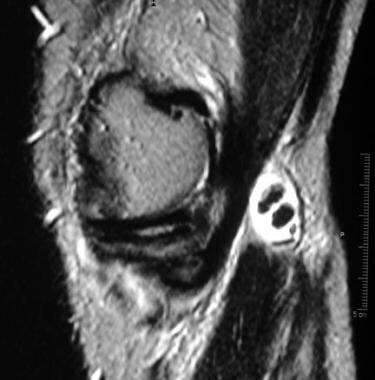
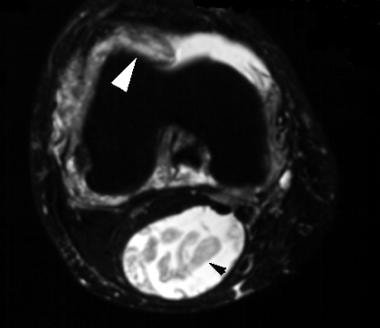 Axial, T2-weighted magnetic resonance image of the knee shows effusion, synovial proliferation (white arrowhead), and a Baker cyst that contains debris (black arrowhead).
Axial, T2-weighted magnetic resonance image of the knee shows effusion, synovial proliferation (white arrowhead), and a Baker cyst that contains debris (black arrowhead).
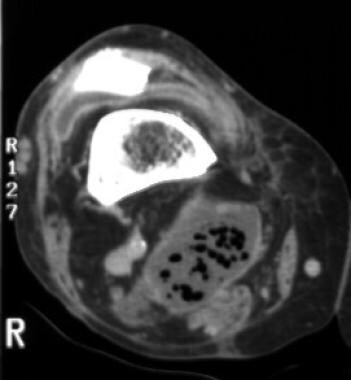 Contrast-enhanced, axial computed tomography (CT) scan of the knee shows multiple gaslike lucencies within a Baker cyst and synovial enhancement.
Contrast-enhanced, axial computed tomography (CT) scan of the knee shows multiple gaslike lucencies within a Baker cyst and synovial enhancement.
Differential diagnosis includes the following:
-
Ganglion cyst [1]
-
Meniscal cyst [11]
-
Myxoid liposarcoma
-
Popliteal artery aneurysm [11]
-
Popliteal artery pseudoaneurysm
-
Synovial sarcoma [12]
-
Osteochondrolipoma [13]
-
Deep vein thrombosis (DVT) [14]
Care must be taken to differentiate ruptured Baker cysts from deep venous thrombosis (DVT). Administration of low-molecular-weight heparin to treat suspected DVT can lead to compartment syndrome
Radiography
Imaging evaluation of a popliteal mass begins with conventional radiography to detect a soft-tissue mass, calcifications, and bony involvement. A Baker cyst appears as a soft-tissue mass in the posteromedial knee joint. [30] Occasionally, a Baker cyst is suggested by the presence of multiple, calcified loose bodies in the cyst (see the images below).
 Anteroposterior radiograph of the knee shows calcifications (arrowhead) overlying the medial tibial plateau.
Anteroposterior radiograph of the knee shows calcifications (arrowhead) overlying the medial tibial plateau.
 Lateral radiograph of the knee shows multiple calcified bodies (arrowhead) posterior to the knee, which is consistent with synovial osteochondromatosis.
Lateral radiograph of the knee shows multiple calcified bodies (arrowhead) posterior to the knee, which is consistent with synovial osteochondromatosis.
Rarely, a solitary loose body in a Baker cyst may mimic a fabella on a lateral radiograph of the knee (see the image below).
 Lateral radiograph of the knee shows a calcified body (arrowhead), which appears to be a large fabella, posterior to the knee.
Lateral radiograph of the knee shows a calcified body (arrowhead), which appears to be a large fabella, posterior to the knee.
However, on a frontal radiograph (see the image below), the calcified body in the Baker cyst will be located behind the medial femoral condyle, whereas a fabella will be present behind the lateral femoral condyle.
 Anteroposterior radiograph of the knee shows that a calcified body (arrowhead) is overlying the medial femoral condyle, making a fabella highly unlikely. The calcified, loose body is in a Baker cyst.
Anteroposterior radiograph of the knee shows that a calcified body (arrowhead) is overlying the medial femoral condyle, making a fabella highly unlikely. The calcified, loose body is in a Baker cyst.
Jayson and Dixon studied the valvular mechanisms in juxta-articular cysts and postulated that joint effusion and fibrin are pumped from the knee joint into the Baker cyst but—because of a valvelike communication (either a Bunsen or ball valve)—not in the reverse direction. [31] The effusion can be readily reabsorbed through the synovial membrane, leaving behind concentrations of fibrin, which on radiographs may appear as gaslike lucencies.
A noninfected Baker cyst with gaslike lucencies (see the images below) may occur along with diabetes mellitus and rheumatoid arthritis (RA). Because gaslike lucencies in a Baker cyst are rare and an infected Baker cyst is a serious condition, the former diagnosis must be one of exclusion; a CT scan with appropriate window settings allows discrimination between air and fibrin.
 Anteroposterior radiograph of the knee shows multiple tiny lucencies superior to the medial femoral condyle (arrowhead).
Anteroposterior radiograph of the knee shows multiple tiny lucencies superior to the medial femoral condyle (arrowhead).
Computed Tomography
On a CT scan, a Baker cyst appears as a fluid-containing mass located behind the medial femoral condyle and between the tendons of the medial head of the gastrocnemius and semimembranosus muscles. A space-occupying lesion in the posteromedial knee suggests the diagnosis but is not always sufficient to exclude other etiologies, for which MRI or ultrasonography is more specific.
CT scanning is not as sensitive as MRI in detecting an internal derangement, which may be the cause of a Baker cyst. In addition, the definitive diagnosis of a Baker cyst may not be made without the injection of air and/or iodinated contrast material into the knee joint (see the image below).
Magnetic Resonance Imaging
On MRI, a Baker cyst appears as a homogeneous, high-signal intensity, cystic mass behind the medial femoral condyle; a thin, fluid-filled neck interdigitates between the tendons of the medial head of the gastrocnemius and semimembranosus muscles (see the image below). [21, 27, 29, 32, 33, 34, 35, 36]
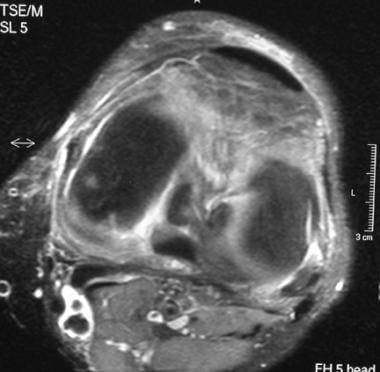
 Axial, T2-weighted magnetic resonance image with fat saturation reveals a Baker cyst connected to the knee joint by way of a narrow neck between the tendons of the medial head of the gastrocnemius and semimembranosus muscles.
Axial, T2-weighted magnetic resonance image with fat saturation reveals a Baker cyst connected to the knee joint by way of a narrow neck between the tendons of the medial head of the gastrocnemius and semimembranosus muscles.
An uncomplicated Baker cyst should demonstrate homogeneous high-signal intensity on all fluid-sensitive pulse sequences, including on the second echo of a conventional or fast/turbo spin-echo sequence, on short tau inversion recovery (STIR), or on gradient echo (GRE)/fast field echo (FFE) sequences employing a low flip angle (10-30º). The axial plane (see the previous image) allows the cyst, neck, and joint space to be seen in contiguity, although the cyst may be demonstrated in all 3 planes.
In addition, intravenously administered gadolinium can detect synovial enhancement (see the images below) and pannus formation in RA in the cyst and in the joint space proper, prior to the radiographic detection of well-known signs of RA much later in the course of the disease (erosion, uniform joint space loss without marked osteophytosis, periarticular osteopenia, soft-tissue swelling).
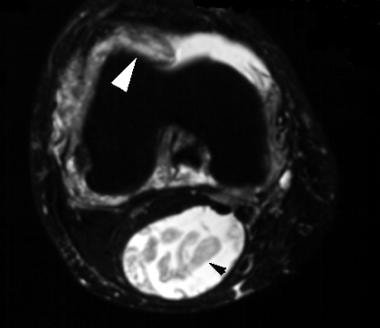 Axial, T2-weighted magnetic resonance image of the knee shows effusion, synovial proliferation (white arrowhead), and a Baker cyst that contains debris (black arrowhead).
Axial, T2-weighted magnetic resonance image of the knee shows effusion, synovial proliferation (white arrowhead), and a Baker cyst that contains debris (black arrowhead).
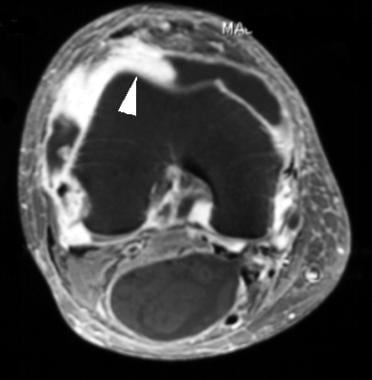 Axial, T1-weighted magnetic resonance image of the knee after the intravenous administration of gadolinium shows synovial enhancement (arrowhead).
Axial, T1-weighted magnetic resonance image of the knee after the intravenous administration of gadolinium shows synovial enhancement (arrowhead).
Off-label usage of intra-articular gadolinium in magnetic resonance arthrography, now common in establishing the presence of a meniscal retear, is perhaps the most vivid way to display a Baker cyst. MRI can also detect underlying internal derangements of the knee (see the images below), which may be etiologic in the formation of a Baker cyst.
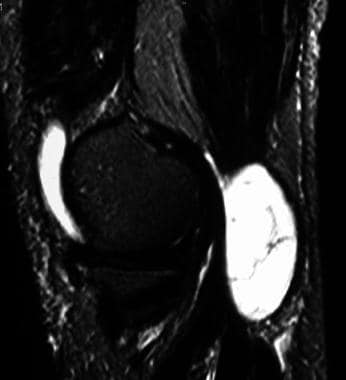
 Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee shows a large knee effusion and a Baker cyst.
Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee shows a large knee effusion and a Baker cyst.
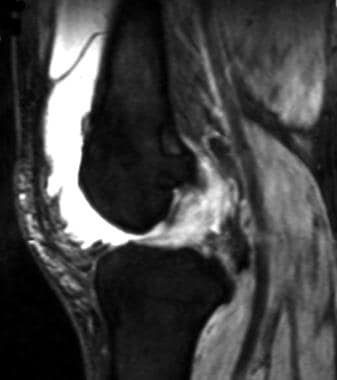 Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee, lateral to the view in Image above, shows a complete rupture of the anterior cruciate ligament.
Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee, lateral to the view in Image above, shows a complete rupture of the anterior cruciate ligament.
In a complex Baker cyst, calcified loose bodies can be detected; these appear on fluid-sensitive images as low-signal intensity, rounded foci within high-signal intensity, cystic fluid (see the images below).
 Sagittal, T2-weighted magnetic resonance image with fat saturation shows a complicated Baker cyst containing multiple internal septations.
Sagittal, T2-weighted magnetic resonance image with fat saturation shows a complicated Baker cyst containing multiple internal septations.
 Sagittal, T2-weighted magnetic resonance image shows a Baker cyst containing hypointense, loose bodies.
Sagittal, T2-weighted magnetic resonance image shows a Baker cyst containing hypointense, loose bodies.
 Axial, T2-weighted magnetic resonance image with fat saturation shows a Baker cyst containing hypointense, loose bodies.
Axial, T2-weighted magnetic resonance image with fat saturation shows a Baker cyst containing hypointense, loose bodies.
Sansone and colleagues reviewed the incidence of associated intra-articular disorders in a series of 1001 adult patients undergoing MRI of the knee and found that the most common associated lesions were meniscal tears, chondral lesions, and ACL tears. [32]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
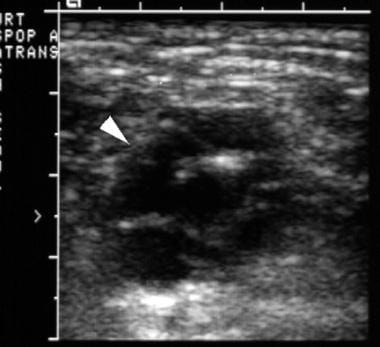
Ultrasonography is a very helpful imaging technique in the evaluation of a popliteal mass. [37, 38, 39, 22, 40, 41, 42] The modality can be used to determine whether the popliteal mass is a cyst or a solid mass. A simple Baker cyst appears as an anechoic mass with posterior acoustic enhancement that communicates with the knee joint. Findings on an ultrasonogram relate to the criteria of a simple cyst, which include an anechoic mass, a sharply defined posterior wall, and posterior acoustic enhancement. A complex Baker cyst has internal echoes within the hypoechoic mass (see the images below).
 Transverse ultrasonographic image of the knee in a patient who had recent arthroscopy shows a complex, cystic mass (arrow) in the medial aspect of popliteal fossa. The mass communicates with the knee joint (arrowhead), which is consistent with a Baker cyst.
Transverse ultrasonographic image of the knee in a patient who had recent arthroscopy shows a complex, cystic mass (arrow) in the medial aspect of popliteal fossa. The mass communicates with the knee joint (arrowhead), which is consistent with a Baker cyst.
 Longitudinal ultrasonographic image of a Baker cyst in a patient who underwent recent knee arthroscopy.
Longitudinal ultrasonographic image of a Baker cyst in a patient who underwent recent knee arthroscopy.
Calcified loose bodies within a Baker cyst appear as mobile, intraluminal, echogenic foci with distal acoustic shadowing, an appearance similar to that of cholelithiasis in a gallbladder. An additional advantage of ultrasonography is that it can exclude a coexisting DVT.
Color Doppler ultrasonography can detect vascular flow within the mass to exclude a popliteal artery aneurysm. In cystic adventitial degeneration of the popliteal artery, ultrasonographic examination reveals multiple cystic structures surrounding a normal-sized artery (see the images below). This is the fastest, most cost-effective manner in which to diagnose a Baker cyst.
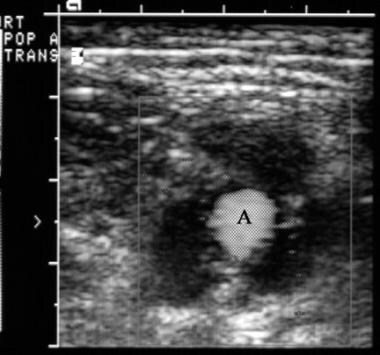 Transverse color Doppler ultrasonographic image of the popliteal fossa shows multiple cysts surrounding a normal-sized popliteal artery (A), which is consistent with cystic adventitial degeneration.
Transverse color Doppler ultrasonographic image of the popliteal fossa shows multiple cysts surrounding a normal-sized popliteal artery (A), which is consistent with cystic adventitial degeneration.
A cyst that is too large or complex may obscure visualization of the fluid-filled connection to the joint space proper, leading to a false-positive diagnosis.
Arthritis is the most common condition associated with Baker cysts, with osteoarthritis probably being the most frequent cause among the arthritides. [24] Although the prevalence of Baker cysts in patients with inflammatory arthritis is higher than in patients with osteoarthritis, osteoarthritis is much more common than inflammatory arthritis. Using ultrasonography, Fam and colleagues found that 21 of 50 patients (42%) with osteoarthritis had Baker cysts. [37] Bilateral cysts were seen in 8 patients (16%). The occurrence of Baker cysts relates directly to the presence of knee effusion and the severity of the osteoarthritis.
In 99 consecutive patients with RA, Andonopoulos and coauthors demonstrated Baker cysts on ultrasonograms of 47 patients (48%). [38] Twenty of the 99 patients (20%) had bilateral cysts. Of 198 knees, 67 (34%) had Baker cysts, yet only 29 cysts (43%) were diagnosed clinically. Baker cysts appear much less frequently in children than in adults. The prevalence of Baker cysts in asymptomatic children examined ultrasonographically was 2.4%. The prevalence of Baker cyst in children undergoing MRI examination of the knee was 6.3%. None of the children with Baker cyst demonstrated an associated ACL or meniscal tear. Four patients (8%) had osteochondritis dissecans (N = 2), septic arthritis (N = 1), or juvenile RA (n = 1). In most children with Baker cysts (82%), the cysts disappeared without intervention (84%) or caused no symptoms (16%). However, in children with arthritis, Baker cysts are common.
In a study of 44 children with knee arthritis, ultrasonography detected a Baker cyst in 27 children (61%), most of whom (80%) had juvenile RA. [39] The remaining causes of arthritis in the study included spondyloarthropathy, psoriatic arthritis, septic arthritis, and systemic lupus erythematosus. Cysts were followed prospectively with serial ultrasonography for 18-24 months. Cysts resolved with the resolution of suprapatellar effusion. Reports of Baker cyst associated with gout, Reiter syndrome, psoriasis, and systemic lupus erythematosus exist. The common underlying pathology for these medical conditions is synovial proliferation with effusion.
In a study by Stroiescu et al of image-guided aspiration followed by therapeutic injection for symptomatic Baker cysts, ultrasonographic and fluoroscopic guidance followed by therapeutic injection of methylprednisolone acetate and bupivacaine was shown to provide durable reduction in pain symptoms in the majority of patients. [5]
In a meta-analysis of 13 studies (1011 patients) regarding the use of ultrasonography to diagnose Baker cyst, sensitivity and specificity were 0.97 and 1.00, respectively, compared to pathology. [16]
-
Valvular mechanism of Baker cyst. Effusion and fibrin are pumped (large arrows) into the Baker cyst (long, thin arrows). In the Bunsen-valve mechanism, the enlarging Baker cyst exerts mass effect (feathered arrow) on the slitlike communication between the joint and the cyst, trapping effusion. In the ball-valve mechanism, fibrin serves as a 1-way valve that prevents the effusion's return to the knee joint. Trapped effusion is reabsorbed through the semipermeable membrane (short, thin arrows), leaving behind concentrations of fibrin. (MFC: medial femoral condyle; MTP: medial tibial plateau; G: medial head of gastrocnemius muscle; SM: semimembranosus muscle)
-
Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
-
Transverse ultrasonographic image of the knee in a patient who had recent arthroscopy shows a complex, cystic mass (arrow) in the medial aspect of popliteal fossa. The mass communicates with the knee joint (arrowhead), which is consistent with a Baker cyst.
-
Longitudinal ultrasonographic image of a Baker cyst in a patient who underwent recent knee arthroscopy.
-
Transverse ultrasonographic image of the popliteal fossa shows a complex, cystic mass (arrowhead).
-
Transverse color Doppler ultrasonographic image of the popliteal fossa shows multiple cysts surrounding a normal-sized popliteal artery (A), which is consistent with cystic adventitial degeneration.
-
Axial, T2-weighted magnetic resonance image with fat saturation reveals a Baker cyst connected to the knee joint by way of a narrow neck between the tendons of the medial head of the gastrocnemius and semimembranosus muscles.
-
Anteroposterior radiograph of the knee shows calcifications (arrowhead) overlying the medial tibial plateau.
-
Lateral radiograph of the knee shows multiple calcified bodies (arrowhead) posterior to the knee, which is consistent with synovial osteochondromatosis.
-
Lateral radiograph of the knee shows a calcified body (arrowhead), which appears to be a large fabella, posterior to the knee.
-
Anteroposterior radiograph of the knee shows that a calcified body (arrowhead) is overlying the medial femoral condyle, making a fabella highly unlikely. The calcified, loose body is in a Baker cyst.
-
Axial, T2-weighted magnetic resonance image of the knee shows effusion, synovial proliferation (white arrowhead), and a Baker cyst that contains debris (black arrowhead).
-
Axial, T1-weighted magnetic resonance image of the knee after the intravenous administration of gadolinium shows synovial enhancement (arrowhead).
-
Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee shows a large knee effusion and a Baker cyst.
-
Sagittal, T2-weighted magnetic resonance image with fat saturation of the knee, lateral to the view in Image above, shows a complete rupture of the anterior cruciate ligament.
-
Sagittal, T2-weighted magnetic resonance image with fat saturation shows a complicated Baker cyst containing multiple internal septations.
-
Sagittal, T2-weighted magnetic resonance image shows a Baker cyst containing hypointense, loose bodies.
-
Axial, T2-weighted magnetic resonance image with fat saturation shows a Baker cyst containing hypointense, loose bodies.
-
Arthrography of the knee performed prior to radioactive synoviorthesis shows leakage of contrast (arrow) just superior to the sinus (arrowhead and "BB" marker).
-
Anteroposterior radiograph of the knee shows multiple tiny lucencies superior to the medial femoral condyle (arrowhead).
-
Lateral radiograph of the knee shows multiple tiny lucencies (arrowhead) posterior to the knee.
-
Contrast-enhanced, axial computed tomography (CT) scan of the knee shows multiple gaslike lucencies within a Baker cyst and synovial enhancement.