Detection of Breast Lesions
As breast cancer screening with mammography increases, many impalpable breast lesions are being detected. [1] These lesions should first and foremost be definitively diagnosed by using image-guided needle biopsy. Thus, breast biopsy with needle localization is used for the diagnosis of impalpable breast lesions. After needle biopsy, some of these lesions may require diagnostic or therapeutic surgical biopsy. If a malignant or indefinite diagnosis is obtained, surgical excision is indicated. This, in turn, requires accurate localization of the lesion, which is required to ensure correct and adequate removal of the lesions and to minimize the degree of cosmetic disfigurement. [2]
The following images depict the localization of masses on mammograms.
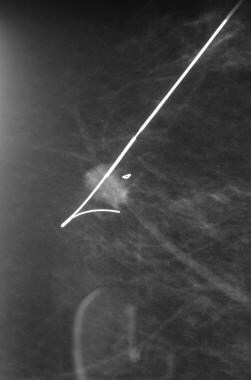 Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
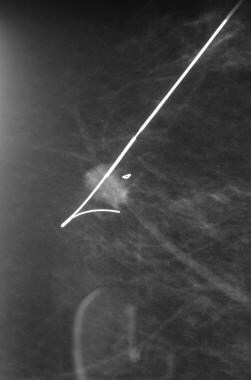
 Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
See Breast Cancer, Ultrasonography in Breast Cancer, and Mammography in Breast Cancer for more information on these topics.
Imaging and Localization Considerations
The modality of choice depends on operator expertise and the type of lesion. Most palpable lesions do not require image-guided localization. Breast lesions that are visible with ultrasonography can be adequately localized by using a skin marker if the lesion lies fairly superficially within the breast. [3] Ultrasound-guided wire localization of biopsy-proven metastatic axillary lymph nodes with clip placement not only significantly improves the success rate of surgical removal but also allows for more accurate staging and reduces the false-negative rates of sentinel node lymph node biopsy following neoadjuvant therapy. [4] In addition, a surgeon can easily perform ultrasonographic localization in the operating room to identify the lesion and to confirm its adequate removal. [5, 6] However, successful preoperative planning for a needle localization procedure—in which lesion location, size, type, and configuration are considered, as well as review of pertinent imaging studies and imaging and pathology reports, particularly pre- and post-biopsy imaging and evaluation of the targeted lesions and the type and position of the marker clips—are essential, as is presurgical communication with the surgeon. [7]
Other localization techniques include magnetic resonance imaging (MRI) and mammography (by using a grid, a holey plate, or a stereotactic method) (see the images below). [8, 9] Although a number of techniques are used to localize nonpalpable breast lesions, needle localization is the most common. [7, 10, 11, 12]
 Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
After successful placement of a guidewire, the patient is then taken to the operating room, where the surgeon commonly makes an incision at the site of the wire insertion and excises the wire and the lesion (see the following images). Some surgeons place a stiff outer cannula along the wire down to the wire tip and excise the tip along with the lesion.
 Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
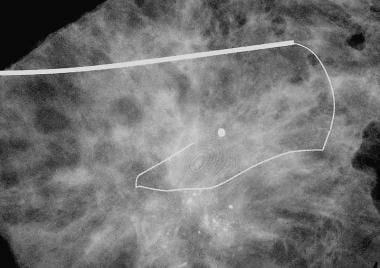
 Breast biopsy with needle localization. The specimen radiograph shows the wire and the localized speculated mass in situ, with a good excision margin.
Breast biopsy with needle localization. The specimen radiograph shows the wire and the localized speculated mass in situ, with a good excision margin.
Impalpable lesions may also be marked by using an injection of methylene blue, [13, 14] charcoal suspension, [15] or radioisotopes. [16]
It is essential to obtain a diagnosis with a core biopsy under ultrasonographic or stereotactic guidance before surgery so that a definitive, one-step surgical procedure can be planned. Once malignancy is diagnosed, any of the following procedures can be used to localize the lesion:
Radiographic Localization
Techniques that involve mammography usually require the upright mammographic attachment on a normal mammographic unit, although localizations with stereotactic prone tables also have been described. Before stereotaxy came into use, a grid (see the image below) or holey plate was used to calculate the position of needle placement in the X and Y planes.
The depth was calculated from the lateromedial projection. The position was then checked according to the superimposition of target, hub, and shaft of the needle, and the required depth was verified on the orthogonal view (see the following image).
 Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
Stereotaxy enables the exact position to be located. The needle is then placed 1 cm beyond the lesion to ensure that it is adequately transfixed. Because of the accordion effect (the thickness of the breast expands when compression is released), the needle tip may migrate, causing the needle to be placed short of the lesion. [17] The final depth of the needle is therefore checked on the orthogonal view to ensure that the lesion is adequately transfixed.
Different needles exist, and most are introduced by using a stiffer, coaxial needle. Some needles are then removed, leaving the wire in situ. The wires commonly have a barb or hook that is deployed in the final position to anchor the wire in place. Some needles require the outer cannula to be retained in situ (see the image below). The choice of needles and wires used are dictated by the preference of the radiologist and the surgeons.
 Breast biopsy with needle localization. This specimen radiograph shows a stellate lesion containing a clustered, pleomorphic microcalcification with wire in situ. Note the use of a stiff outer cannula.
Breast biopsy with needle localization. This specimen radiograph shows a stellate lesion containing a clustered, pleomorphic microcalcification with wire in situ. Note the use of a stiff outer cannula.
After surgical removal of the lesion, specimen radiography must be performed to ensure that the lesion was adequately excised (see the following image).
 Breast biopsy with needle localization. The specimen radiograph shows the wire and the localized speculated mass in situ, with a good excision margin.
Breast biopsy with needle localization. The specimen radiograph shows the wire and the localized speculated mass in situ, with a good excision margin.
Note that architectural distortion on mammograpthy may also pose a challenge in radiologic-pathologic correlation. In a retrospective case series comprising data from 588 core needle biopsies over 6 years, investigators found about one third of these biopsies for lesions associated with architectural distortion identified predominantly invasive, low-grade, ER+, HER2–, and low-stage carcinomas. [18] Moreover, there were differences between single-feature and multi-feature architectural distortions owing to fewer carcinomas on core needle biopsy (18% vs 39%, respectively), and the identification of undetected invasive carcinomas in the latter group. The investigators indicated that nonspecific findings on core needle biopsy will remain challenging for correlating radiology-pathology findings as well as decision making on excision recommendations in some patients with multi-feature architectural distortion. [18]
Magnetic Resonance Imaging Localization
The use of magnetic resonance imaging (MRI) localization reflects the increasing use of magnetic resonance mammography. [19] Although a portion of MRI-depicted lesions can subsequently be localized with ultrasonography, some of them are mammographically and ultrasonographically occult, which means that they require MRI-guided needle biopsy or localization. [8, 19, 20]
All of the major manufacturers of MRI units have made biopsy attachments available; these require the patient to be kept in a semiprone position. MRI is then performed with the intravenous administration of a gadolinium-based contrast agent, and the lesion is localized by using MRI-compatible localization needles. [21] The correct placement of the needle can be confirmed by obtaining a T2-weighted MRI to verify the signal void to transfix the lesion.
Technical challenges
Technical difficulties and challenges include the tendency of the MRI-visible lesion to fade over time (because enhancement with contrast material is transient). [8] In addition, because of the amount of time required to perform the procedure (30-60 min), the patient may begin to move, which could cause an error in needle placement. Nevertheless, MRI localizations have generally been as accurate as mammographic localizations, with miss rates of 2-9%. Some investigators have suggested that postoperative MRI should be performed to verify complete excision of the lesion.
Gadolinium warning
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans.
NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonographic Localization
When the breast lesion is visible, ultrasonography is the modality of choice for needle placement (see the following image). This technique provides the advantage of real-time imaging, allowing accurate placement of the needle. Being able to directly visualize the lesion and needle position results in a quicker procedure, reducing the risk of patient morbidity. As in mammographic techniques, the lesion must be transfixed, and orthogonal mammography can be used to confirm that the correct lesion has been localized.
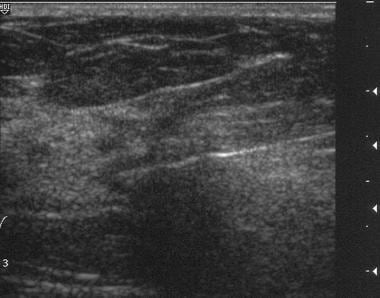 Breast biopsy with needle localization. This figure shows a poorly attenuating lesion being transfixed with a hook wire under ultrasonographic guidance.
Breast biopsy with needle localization. This figure shows a poorly attenuating lesion being transfixed with a hook wire under ultrasonographic guidance.
The use of intraoperative ultrasonography by the surgeon in the operating theater, as well as the employment of skin marking, is described in the Imaging and Localization Considerations section, above.
Nuclear Medicine Localization
Nuclear medicine study was originally used for sentinel lymph node biopsy (SLNB). Colloidal albumin labeled with technetium-99m (99m Tc) is injected directly into the lesion under stereotactic or ultrasonographic guidance. [16]
The accuracy of isotope placement is checked with scintigraphy. Excision biopsy is then performed by using a gamma probe. After excision, the excised lesion and the cavity are checked for radioactivity, and the specimen is radiographed to ensure the radiographic adequacy of the excision. Results from a study of 67 consecutive patients showed complete removal of the lesion in 99.5% of them. [22] Thus, this technique is accurate and at least comparable to conventional wire localization.
Radiation exposure
Measured radioactive doses to the breast (0.03 ± 0.02 mGy/MBq) and to the surgeon's hand (7.5 ± 5.0 µSv/h) appear to be negligible. [22]
Tissue Excision
The amount of tissue that is excised is dependent on the nature of the surgical procedure. If a diagnostic procedure is performed, a small volume of tissue is removed so that histologic diagnosis can be achieved with minimal scarring. When surgery is performed to treat malignant disease, the aim is to excise the lesion with a clear margin in order to minimize the risk of local recurrence. [16]
Complications
All localization methods are subject to potential inaccuracies. [17] It is important to confirm the correct placement of the guidewire. Ultrasonographic and mammographic wire localizations can be followed by mammography performed in two planes (eg, lateromedial and craniocaudal projections) to confirm that the correct lesion has been accurately targeted.
Ideally, the guidewire should transfix the lesion on both projections (see the image below). The tip of the guidewire should ideally be placed within 1 cm of the target lesion.
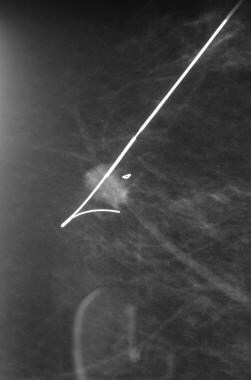 Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
Guidewires may be dislodged or may migrate before surgery. Complications, including pneumothoraces, have been described. Wire fragments may also be retained following surgery. Published literature show that the rate of needle-localization failure is in the range of 0-20%. Factors associated with such failure include the following [23, 24, 25] :
-
Lesion type
-
Lesion size
-
Increased distance of the needle from the lesion
-
Decreased breast size
-
Decreased specimen volume
Stereotactic core needle breast biopsy markers may also migrate (about 13% in a study [26] ) Factors that contribute to marker migration include global fatty breast density and biopsy in the inner region of the breast, whereas a superior biopsy approach, locally heterogeneous breast density, and T-shaped biopsy markers do not appear to be associated with marker migration. [26]
Another potential concern is the risk of needle tract seeding or tumor cell dissemination during breast needle biopsy procedures. A 2024 literature review by Holmes indicates that it is common for needle-biopsy-induced cell displacement to occur, impacted by factors such as the biopsy technique and type of breast cancer, possibly raising the risk of local recurrence (but without affecting regional recurrence and long-term survival). [27]
-
Breast biopsy with needle localization. This mammogram shows a spiculated mass to be transfixed by the guidewire.
-
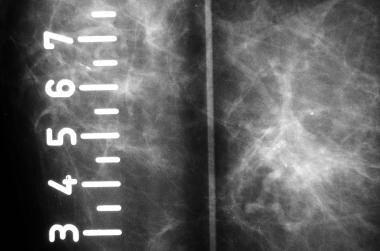
Breast biopsy with needle localization. The grid technique of localization is demonstrated.
-
Breast biopsy with needle localization. This orthogonal (mediolateral) projection confirms the position of the needle to be placed beyond the cluster of microcalcification.
-
Breast biopsy with needle localization. The specimen radiograph shows the wire and the localized speculated mass in situ, with a good excision margin.
-
Breast biopsy with needle localization. This figure shows a poorly attenuating lesion being transfixed with a hook wire under ultrasonographic guidance.
-
Breast biopsy with needle localization. This specimen radiograph shows a stellate lesion containing a clustered, pleomorphic microcalcification with wire in situ. Note the use of a stiff outer cannula.