Background
Soft tissue knee injuries are some of the most common and clinically challenging musculoskeletal disorders seen in the emergency department (ED). Accurate and timely diagnosis increases the likelihood of fully restoring normal and pain-free use of the affected knee.
Knee pain and related symptoms may derive from damage to one or more of the soft tissue structures that stabilize and cushion the knee joint (including the ligaments, muscles, tendons, and menisci), from infection to the knee joint or surrounding structures, or from trauma to the bones forming the joint. In addition to the etiology of the patient's presenting symptoms, determine the acuity of the pathologic process as an acute traumatic or infectious event or exacerbation of a chronic overuse or degenerative syndrome. [1, 2, 3]
For most patients, the severity of the etiology and the injury or pathologic process, acute or chronic, can be determined from a targeted history, focused physical examination, and thoughtful workup including diagnostic imaging (eg, plain radiography).
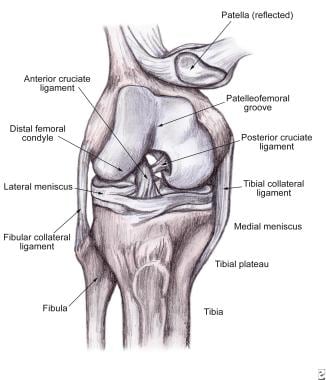
The image below depicts the normal anatomy of the knee.
Pediatric patients
In any child with a traumatic injury, be alert to the possibility of child abuse.
Children with hip disorders, especially a slipped capital femoral epiphysis and Legg-Calvé-Perthes disease, may have referred pain to the knee. Ligamentous damage, meniscal damage, and dislocations (with the exception of patellar dislocations) are rare in children.
Children with open epiphyseal plates may have injuries that can be mistaken for soft tissue injuries. The missing of growth-plate injuries in children may result in deformity and growth irregularities. If the patient has circumferential tenderness about the lower part of the femur or the proximal tibia, treat it as a Salter-Harris growth-plate injury, even if radiography findings are normal.
In young patients who are skeletally immature, measurement of skeletal age with an anteroposterior radiograph of the left hand and wrist and Tanner stage may help guide treatment. [4]
Impetuous stress testing of the knee joint may induce additional damage, displacing a fracture or worsening a growth-plate disturbance.
A completely displaced epiphyseal fracture of the distal femur is the pediatric equivalent of adult knee dislocation. This injury may also harm the popliteal artery.
Osteochondritis dissecans, an intra-articular disorder of unclear etiology, is most common in boys during late childhood or in male adolescents. The condition is characterized by degeneration and recalcification of the articular cartilage and underlying bone. Patients tend to report vague, poorly localized knee pain, as well as morning stiffness or recurrent effusions. Osteochondritic lesions can be radiographically occult, and computed tomography (CT), bone scanning, or magnetic resonance imaging (MRI) may be required to make the diagnosis.
Although not strictly a disease, Osgood-Schlatter disease probably originates from microtrauma, leading to apophysitis at the insertion of the patellar tendon into the tibial tubercle.
Complaints of knee pain generally start in energetic children aged 9-15 years, a time of rapid growth. Discomfort tends to be localized, and palpation reveals swelling and tenderness over the tibial tubercle. Boys are affected more commonly than girls; activity exacerbates pain, and bilateral involvement occurs in about 30% of patients.
Initial treatment is conservative, with activity limited to the patient's tolerance.
Geriatric patients
Rupture of the extensor mechanism may precede trivial trauma in the elderly, especially in individuals with coexisting disorders, such as renal failure, systemic lupus erythematosus, hyperparathyroidism, or diabetes mellitus.
Because of underlying degenerative disease, meniscal tears may emerge in older patients with a history of minimal or no trauma. For example, simply rising from a squatting position may cause a tear.
Discomfort and distention related to the knee after a fall may arise from a fracture of the tibial plateau, especially the lateral plateau.
Osteoporosis, commonly occurring in elderly persons, makes bones more vulnerable to fracture. Visualization of fractures on plain images is difficult, and fractures may be easily overlooked. Misdiagnosing this fracture as a soft tissue injury may lead to additional morbidity, as fracture fragments may be displaced.
Pregnant patients
Knee problems, especially underlying meniscal and patellar problems, may worsen with pregnancy because of changes in the biomechanics of weight bearing and shifting in the center of gravity with fetal development.
Production of relaxin hormone during pregnancy may modify ligaments of the knee, in addition to those of the pelvis, increasing knee laxity.
Radiography in pregnancy is always a concern. Although some risk is associated with obtaining diagnostic radiographs in pregnancy, animal and human data do not reveal an increased risk to the fetus when fetal exposure is limited. After 20 weeks' gestation, the risk of radiation exposure that might cause fetal abnormalities is remote; however, avoid unessential radiography. If radiographs are deemed indispensable, shield the patient's abdomen.
Pathophysiology
To understand the various injury patterns associated with trauma to the knee, understanding the anatomy is important. The anatomy of the knee is shown in the image below. Knee symptoms arise from an alteration or disruption of the normal anatomic structures that impede normal knee function. In mechanical terms, the knee performs like a rolling cam rather than as a simple hinged (ginglymus) joint. As the knee proceeds from flexion to extension, a complex screw-type of motion takes place, with the femoral condyles locking into the tibial plateau as the femur rotates internally. Full knee extension increases the tautness of the major bracing ligaments, transforming the knee into a mechanically rigid structure. Flexion loosens the knee joint by unlocking and disengaging the bracing structures, including retraction of the menisci, thereby enhancing ligamentous laxity and increasing the range of motion (ROM) of the joint.
Two separate but interdependent joints forming the knee are the tibiofemoral articulation and the patellofemoral coupling. Weight-bearing forces, as much as 5 times an individual's body weight, are transmitted through the opposing condyles of the femur and the tibia. Two shock-absorbing cartilaginous menisci interpose between the femur and the tibia, forming the largest synovial joint in the body. The medial meniscus is smaller and more fixed than the lateral meniscus; these features predispose it to injury. A fibrous capsule lined by a synovial membrane also surrounds and bolsters the knee joint but does not contribute to the inherent stability of the joint.
Fitness of the knee joint largely depends on the fortifying ligaments and muscles binding together the femur, tibia, and patella. Two sets of knee ligaments are frequently affected. The first set, lying outside of the knee joint proper, are the extracapsular collateral ligaments. These ligaments consist of the medial collateral ligament (MCL), which opposes extreme abductive and/or valgus forces, and its counterpart, the lateral collateral ligament (LCL), which limits excessive adductive and/or varus pressures. The second set, crisscrossing in the knee joint, are the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), which individually brace against excessive translation in the anteroposterior (AP) plane. The ACL serves as the primary knee stabilizer, preventing forward displacement of the tibia on the femur.
Primarily formed by the quadriceps muscles, the extensor apparatus envelops and stabilizes the patella. At its distal aspect, the quadriceps muscle consolidates into the patellar ligament, ultimately inserting onto the tibial tubercle. Several bursae envelop the knee, including the prepatellar, superficial and deep infrapatellar, and pes anserine bursae, which permit friction-free movement between the various structures. Acute trauma or repetitive occupational stress may incite inflammation; infection and metabolic disorders (eg, gout) are less common etiologies. Inflammation of the bursa then leads to localized tenderness, erythema, and increased warmth. Extensive bursae in this area alleviate potentially damaging frictional forces between the susceptible structures. Fixed in the back of the knee joint, in the popliteal fossa, are vital neurovascular structures, including the popliteal artery.
Definitions and grades of sprains and strains
Sprains to the knee are characterized by the stretching or tearing of noncontractile structures, such as the investing ligaments or of the joint capsule itself, whereas a strain refers to stretching or severing along the course of muscles or tendons. Both collateral ligament and cruciate ligament sprains, as well as muscular strains, are relatively common. Ligamentous (sprain) and muscular (strain) injuries may be classified according to the degree of impairment.
-
Grade I sprain - Stretching but no tearing of the ligament, local tenderness, minimal edema, no gross instability with stress testing, firm end point
-
Grade II sprain - Partial tears of the ligaments, moderate local tenderness, mild instability with stress testing (but firm end point), moderately incapacitating
-
Grade III sprain - Complete tear, discomfort with manipulation but less than expected for degree of injury, variable amount of edema (ranging from negligible to grossly conspicuous), clear instability with stress testing (expressing a mushy end point), severe disability
Specific injuries
ACL injury: Rupture of the ACL is among the most serious of the common knee injuries and results from a variety of mechanisms. Most patients with ACL damage complain of immediate and profound pain, exacerbated with motion, and inability to ambulate. Disruption of the ACL may occur alone or with other knee injuries, especially a meniscal injury or tear of the MCL.
PCL injury: Patients typically report falling on a flexed knee or sustaining a direct blow to the anterior aspect of the knee (eg, when the knee strikes the dashboard in a motor vehicle accident). PCL harm signifies a major injury and rarely occurs as an isolated injury.
Etiology
Intrinsic knee injuries
The intrinsic structural framework of the knee and its exposure to the environment account for particular injuries. Harm may arise from direct impact, such as in contact or collision sports or blows to the knee connected to motor vehicle accidents.
Most soft tissue injuries sustained by the knee do not, however, involve direct trauma but arise from actions producing excessive torque on the knee joint, especially those activities involving twisting, rapid deceleration, or landing from a jump. If tensile forces placed on the knee exceed the intrinsic tone of the ligaments, injury to the ligaments results. Low-intensity forces may provoke a reversible injury, with only transient deformation of the elastic ligament; however, profound loads applied to the knee joint produce irreversible rupture of the ligament fibers.
Valgus-directed blows sustained by the externally rotated knee occur commonly.
High-intensity impact to the lateral side of the knee tends to be serious and befalls skiers when catching a ski tip or football players following a blind-side clipping type of injury.
Valgus contact injuries may cause a series of injuries to the knee, including a tear of the MCL, followed by damage to the posterior medial capsule, and, finally, damage to the ACL. This combination of injuries is referred to as O'Donahue or unhappy triad.
An intense varus stress to the knee joint gives rise to a sequence of injuries, depending on the position of the knee.
Impact to the medial side of the knee in a neutral position causes disruption of the LCL, the iliotibial band, and/or the biceps femoris.
Profound varus strain to the extended and internally rotated knee may harm not only the LCL and the ACL, but also the PCL and the lateral posterior capsule.
Undue varus stress to the flexed and internally rotated knee brings about LCL injury, proceeding to damage of the lateral posterior capsule and/or lateral meniscus and, if extreme, impairment of the PCL.
Extensor injuries
Extensor-mechanism injuries result from direct or indirect forces. Direct injuries result from a blow to the anterior aspect of the knee, often causing the patella to fracture. Indirect injury occurs when forced flexion of the knee occurs against a contracted quadriceps.
Depending on the patient's age and the type of force applied, disruption of the extensor mechanism can occur by means of quadriceps tendon tear, patellar fracture, rupture of the patellar tendon, or avulsion of the tibial tuberosity.
Many conditions have been reported to be associated with rupture of the quadriceps tendon, including hyperparathyroidism, chronic renal failure, gout, obesity, leukemia, rheumatoid arthritis, diabetes, systemic lupus erythematosus, steroid use (both local injection and systemic use), and fluoroquinolone use. A considerable delay may exist between the administration of a fluoroquinolone and the spontaneous rupture of a tendon.
Bilateral simultaneous ruptures of the quadriceps tendon are rare, but they have been reported numerous times in the literature. In one series of bilateral quadriceps rupture, 41 (65%) were attributed to falls or missteps, and 22 (35%) occurred spontaneously while the patient was walking. [5]
Patients with meniscal injuries frequently report pain after twisting (rotational force) their knee while bearing weight on the affected side.
Imposing extreme hyperextension force may disrupt the cruciate ligaments, conceivably anywhere along their span.
Rupture of the ACL is among the most serious of the common knee injuries and results from various mechanisms. ACL tears are associated with anterior blows that hyperextend the knee, excessive noncontact hyperextension of the knee, and extreme deceleration forces to the knee. Disruption of the ACL may occur alone or with other knee injuries, especially a meniscal or MCL tear.
Patients with PCL tears typically report falling on a flexed knee or sustaining a direct blow to the anterior aspect of the knee (eg, when the knee strikes the dashboard in an motor vehicle accident). PCL harm signifies a major injury and rarely occurs as an isolated injury.
Epidemiology
Knee pain is a complaint in up to 20% of the general adult population, accounting for almost 3 million outpatient and emergency department visits per year. Trauma to the knee is the second most common occupational accident. The MCL is the most frequently injured ligament in the knee. ACL damage causes the highest incidence of pathologic joint instability.
In a series of 240 patients assessed for meniscus and cruciate ligament lesions of the knee, medial meniscus (MM) lesions were the most common finding (63%), followed by osteoarthritis (48%) and ACL lesions (35%); the majority of the MM and ACL lesions were tears (54.6% and 69.41%). [6]
In National Collegiate Athletic Association (NCAA) football, one major knee injury occurs per team every year. [7] Sports-related activity accounts for approximately 60% of knee injuries producing ligamentous laxity.
In a study of patients with sport-related knee strain and sprain presenting to US emergency departments, the highest injury rates occurred in football and basketball for males and in soccer and basketball for females; the population most at risk was individuals of both sexes aged 15 to 19 years. [1]
Prognosis
Most grade I or II collateral ligament sprains heal uneventfully after a 4- to 6-week course of conservative therapy; however, patients may have chronic pain and a tendency for recurrent injury. Grade III collateral sprains invariably give rise to tears of the posterior capsule, and patients frequently require bracing and physical therapy for 3 months or longer before returning to unrestricted activity.
Outlook for ACL injuries depends on numerous factors, including extent of the lesion, age, activity level desired, and presence of coexistent injuries.
A high rate of recurrence follows simple aspiration of a Baker cyst, while these cysts reappear in less than 5% of cases after surgical correction.
Infection and chronic weakness of the extensor apparatus may follow surgical repair.
Development of recurrent locking, popping, or effusions subsequent to an adequate trial of conservative therapy for meniscal tears may suggest the need for surgical intervention.
Morbidity/mortality
Patients receiving inappropriate or ill-timed care of knee dislocations may have undue morbidity (eg, amputation) due to vascular complications in the distal leg. Oversight of the magnitude of soft tissue injuries of the knee may result in a failure to expeditiously consider compartment syndrome and its resultant complications, including loss of a limb. Misdiagnosis or mismanagement of damage to supporting structures of the knee may lead to chronic knee instability, with subsequent development of degenerative joint disease and/or loss of knee function, including but not limited to an inability to bear weight or ambulate.
Disorders of the patella and lateral meniscus are generally more common in girls and women than in boys and men. Some studies suggest that females are more prone to ACL injuries, which is believed to be due to the fact that the female ACL is both structurally weaker and has a relatively smaller cross-sectional diameter. Chondromalacia patellae or patellar malalignment syndrome (ie, premature erosion and degeneration of patellar cartilage) predominates in young women.
Larsen-Johansson disease of the patella, also known as inferior pole patellar chondropathy, is 9 times more prevalent in boys and men than in girls and women, especially in boys aged 10-14 years.
Ligamentous and meniscal injuries are most likely in young to middle-aged adults, whereas children and adolescents are most susceptible to osseous damage. Most patients with a meniscal tear are aged 20-30 years, but a second peak occurs in patients older than 60 years. Meniscal injuries are rare in children younger than 10 years with morphologically normal menisci.
In general, knee dislocations arise from high-energy trauma, such as motor vehicle accidents. [8]
Overall, 18.1% of US men and 23.5% of US women aged 60 years and older reported knee pain on most days for 6 weeks prior to their medical examination. Additionally, elderly patients may sustain fractures after minimal trauma that typically produces only soft tissue injuries in younger patients.
The region of the extensor mechanism susceptible to disruption is correlated with the patient's age. The older the patient, the more proximal the area of rupture. Disruption of the quadriceps tendon most often occurs in elderly patients, whereas more distal severance of the patellar tendon and avulsion of the tibial tubercle occurs in younger patients.
Complications
Specific dislocations and fractures predispose the knee to popliteal artery and/or peroneal nerve damage.
Significant soft tissue injuries of the knee and lower leg put the lower leg at risk for compartment syndrome.
Knee joint instability may follow unrecognized ligament damage.
Complications of anterior cruciate ligament (ACL) injuries include abnormal knee motion, which eventually causes major degenerative changes in the knee joint. A meta-analysis by Webster and Hewett found a nearly sevenfold increased risk of developing knee osteoarthritis after ACL injury. [9]
Recurrent locking, damage to the articular cartilage, and ensuing arthritis may follow missed meniscal injuries.
Infection may arise from abrasions, lacerations, aspiration, or injection of the knee. If unrecognized, knee joint destruction results.
Spontaneous rupture of tendons may follow use of intra-articular corticosteroids.
-
Anatomy of the knee.
-
Knee ballottement.
-
Lachman test.
-
Anterior drawer sign.
-
Pivot test.
-
McMurray test.
-
Apley compression test.