Practice Essentials
Hypogonadism refers to a condition in which little or no hormone is produced by the testes or ovaries. The condition can be hypergonadotropic (primary, resulting when the gonads fail) or hypogonadotropic. The latter can result from failure of the hypothalamic luteinizing-hormone releasing hormone [LHRH] pulse generator or from the inability of the pituitary to respond with secretion of luteinizing hormone [LH] and follicle-stimulating hormone [FSH]. (See the image below.) Morbidity for men and women with hypogonadism includes infertility and an increased risk of osteoporosis; there is no increase in mortality.
Causes of hypogonadism
Hypogonadotropic hypogonadism can result from the following:
-
Central nervous system (CNS) disorders - Including tumors and miscellaneous causes involving the pituitary/hypothalamic area
-
Genetic causes - Eg, Kallmann syndrome
-
Congenital disorders - Eg, Prader-Willi syndrome, Laurence-Moon syndrome, Bardet-Biedl syndrome, [1] and Gaucher disease
-
Acquired disorders - Eg, exercise-induced hypogonadism, psychogenic hypogonadism, hyperprolactinemia, Cushing syndrome, human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), morbid obesity, type II diabetes mellitus
Causes of hypergonadotropic hypogonadism (primary hypogonadism) in males include the following:
-
Klinefelter syndrome
-
Inactivating mutation
-
Chemotherapy
-
Radiation therapy
-
Gonadectomy
-
Anorchism and cryptorchidism
-
Testicular biosynthetic defects - 17β-hydroxylase dehydrogenase deficiency, 5α-reductase deficiency, 17-hydroxylase deficiency
-
Defects in testicular determination - Gonadal dysgenesis
-
Other rare disorders of
Background
Hypogonadism manifests differently in males and in females before and after the onset of puberty. [6] If onset is in prepubertal males and testosterone replacement is not instituted, the individual has features of eunuchoidism, which include sparse body hair, poor development of skeletal muscles, and delay in epiphyseal closure, resulting in long arms and legs. When hypogonadism occurs in postpubertal males, lack of energy and decreased sexual function are the usual concerns. In females with hypogonadism before puberty, failure to progress through puberty or primary amenorrhea is the most common presenting feature. When hypogonadism occurs in postpubertal females, secondary amenorrhea is the usual concern.
Pathophysiology
The gonads (ovaries or testes) function as part of the hypothalamic-pituitary-gonadal axis. A hypothalamic pulse generator resides in the arcuate nucleus, which releases luteinizing hormone (LH)-releasing hormone (LHRH), which is also termed gonadotropin-releasing hormone (GnRH), into the hypothalamic-pituitary portal system. Data suggest that a gene named KISS is important in the development of the LHRH-secreting cells. [7, 8]
In response to these pulses of LHRH, the anterior pituitary secretes follicle-stimulating hormone (FSH) and LH, which, in turn, stimulate gonadal activity. The increase in gonadal hormones results in lowered FSH and LH secretion at the pituitary level, completing the feedback loop. In the testes, LH stimulates Leydig cells to secrete testosterone, whereas FSH is necessary for tubular growth. In the ovaries, LH acts on theca and interstitial cells to produce progestins and androgens, and FSH acts on granulosa cells to stimulate aromatization of these precursor steroids to estrogen.
Hypogonadism may occur if the hypothalamic-pituitary-gonadal axis is interrupted at any level. Hypergonadotropic hypogonadism (primary hypogonadism) results if the gonad does not produce the amount of sex steroid sufficient to suppress secretion of LH and FSH at normal levels. Hypogonadotropic hypogonadism may result from failure of the hypothalamic LHRH pulse generator or from inability of the pituitary to respond with secretion of LH and FSH. Hypogonadotropic hypogonadism is most commonly observed as one aspect of multiple pituitary hormone deficiencies resulting from malformations (eg, septooptic dysplasia, other midline defects) or lesions of the pituitary that are acquired postnatally. In 1944, Kallmann and colleagues first described familial isolated gonadotropin deficiency. Recently, many other genetic causes for hypogonadotropic hypogonadism have been identified.
Normosmic hypogonadotropic hypogonadism, in which the sense of smell is not disrupted, has been associated with mutations in GNRH1, KISS1R, and GNRHR genes. Although their exact functions are unclear, the genes TAC3 and TACR3 have also been associated with normosmic hypogonadotropic hypogonadism. Kallmann syndrome (anosmic hypogonadotropic hypogonadism) has been associated with mutations in KAL1, FGFR1, FGF8, PROK2, and PROKR2 genes. The relationship with Kallmann syndrome is thought to be because these genes are all related to the development and migration of GnRH neurons. Mutations of an additional gene, CHD7, which has been associated with CHARGE syndrome, has also been found in patients with normosmic or anosmic hypogonadotropic hypogonadism.
Frequency
In women with hypergonadotropic hypogonadism (ie, gonadal failure), the most common cause of hypogonadism is Turner syndrome, which has an incidence of 1 case per 2,500-10,000 live births. In men with hypergonadotropic hypogonadism, the most common cause is Klinefelter syndrome, which has an incidence of 1 case per 500-1000 live births. Hypogonadotropic hypogonadism is rarer.
A study by Livingston et al found that among men whose testosterone levels were checked in primary health-care exams, potential hypogonadism was found in a significant minority. The investigators reported a total testosterone level of under 10 nmol/L in 1924 out of 8788 men (21.9%) in whom testosterone results were determined. [9]
Epidemiology
No racial predilection has been described.
Hypergonadotropic hypogonadism is more common in males than in females because the incidence of Klinefelter syndrome (the most common cause of primary hypogonadism in males) is higher than the incidence of Turner syndrome (the most common cause of hypogonadism in females). Incidence of hypogonadotropic hypogonadism is equal in males and females.
Hypogonadism may occur at any age; however, consequences differ according to the age at onset. If hypogonadism occurs prenatally (even if incomplete), sexual ambiguity may result. If hypogonadism occurs before puberty, puberty does not progress. If hypogonadism occurs after puberty, infertility and sexual dysfunction result.
Prognosis
No increase in mortality is observed in patients with hypogonadism. Morbidity for men and women includes infertility and an increased risk of osteoporosis. In women, an increased risk of severe osteoporosis is noted. In men, hypogonadism causes decreased muscle strength and sexual dysfunction.
Men and women with hypogonadism can lead a normal life with hormone replacement.
Approximately 10-20% of females with Turner syndrome have some spontaneous puberty. Spontaneous estrogenization occurs more commonly in women with mosaic karyotypes and those karyotypes with an abnormal second X chromosome, such as 46,XXiq or 46,XXip. Reports exist of women with mosaic Turner syndrome becoming pregnant without in vitro fertilization.
A multicenter, international, cross-sectional study by Dwyer et al indicated that in males with congenital hypogonadotropic hypogonadism, certain predictors suggest whether or not a patient will experience spontaneous reversal of the hypogonadism after treatment. The investigators found it more likely that anosmia, cryptorchidism, complete absence of puberty (testicular volume < 4 cm3), and at least two rare genetic variants (ie, oligogenicity) would exist in males who do not undergo reversal. In those study patients who were genetically tested, none who experienced reversal had a rare pathogenic form of the ANOS1 gene, compared with 10.5% of those who did not undergo reversal, while those in the reversal group did demonstrate a significantly greater rate of rare variants in the GNRHR gene (12.0% of tested patients) than did the non-reversal patients (3.2% of tested patients). [10]
Patient Education
For patient education resources, see the Men's Health Center and Women's Health Center, as well as Impotence/Erectile Dysfunction and Amenorrhea.
-
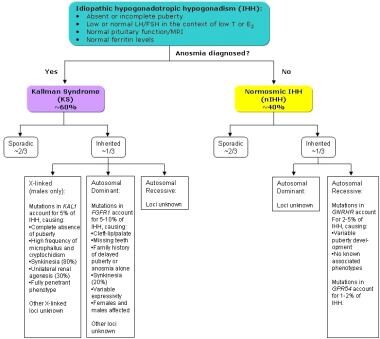
Types of idiopathic hypogonadotropic hypogonadism.