Practice Essentials
Benign paroxysmal positional vertigo (BPPV) is defined as an abnormal sensation of motion that is elicited by certain critical provocative positions. The provocative positions usually trigger specific eye movements (ie, nystagmus). The character and direction of the nystagmus are specific to the part of the inner ear affected and the pathophysiology.
BPPV is probably the most common cause of vertigo in the United States. It has been estimated that at least 20% of patients who present to the physician with vertigo have BPPV. However, because BPPV is frequently misdiagnosed, this figure may not be completely accurate and is probably an underestimation. Since BPPV can occur concomitantly with other inner ear diseases (for example, one patient may have both Ménière disease and BPPV at once), statistical analysis may be skewed toward lower numbers. [1]
BPPV was first described by Barany in 1921. The characteristic nystagmus and vertigo associated with positioning changes were attributed at that time to the otolithic organs. In 1952, Dix and Hallpike performed the provocative positional testing named in their honor, shown below. They further defined classic nystagmus and went on to localize the pathology to the proper ear during provocation.
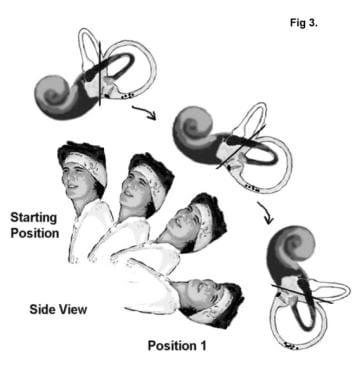 The patient is placed in a sitting position with the head turned 45° towards the affected side and then reclined past the supine position.
The patient is placed in a sitting position with the head turned 45° towards the affected side and then reclined past the supine position.
BPPV is a complex disorder to define; because an evolution has occurred in the understanding of its pathophysiology, an evolution has also occurred in its definition.
Pathophysiology
To understand pathophysiology, an understanding of normal SCC anatomy and physiology is necessary. Each inner ear contains 3 SCCs oriented in 3 perpendicular planes; the SCCs mediate spatial orientation. Each canal consists of a tubular arm (crura) that sprouts from a large barrellike compartment, much like the handle of a coffee mug sprouts from the mug. Each of these arms has a dilated (ampullary) end located near the top or front portion that houses the crista ampullaris (nerve receptors).
The crista ampullaris has a sail-like tower, the cupula, that detects the flow of fluid within the SCC. If a person turns suddenly to the right, the fluid within the right horizontal canal lags behind, causing the cupula to be deflected left (toward the ampulla, or ampullopetally). This deflection is translated into a nerve signal that confirms the head is rotating to the right.
In simple terms, the cupula acts as a 3-way switch that, when pressed one way, appropriately gives the body a sensation of motion. The middle or neutral position reflects no motion. When the switch is moved the opposite way, the sensation of motion is in the opposite direction.
Particles in the canal slow and even reverse the movement of the cupula switch and create signals that are incongruous with the actual head movements. This mismatch of sensory information results in the sensation of vertigo.
Cupulolithiasis theory
In 1962, Harold Schuknecht, MD, proposed the cupulolithiasis (heavy cupula) theory as an explanation for BPPV. Via photomicrographs, he discovered basophilic particles or densities that were adherent to the cupula. He postulated that the posterior semicircular canal (PSC) was rendered sensitive to gravity by these abnormal dense particles attached to or impinging upon the cupula.
This theory is analogous to the situation of a heavy object attached to the top of a pole. The extra weight makes the pole unstable and thus harder to keep in the neutral position. In fact, the pole is easily prone to "clunk" from one side to the other depending on the direction it is tilted. Once the position is reached, the weight of the particles keeps the cupula from springing back to neutral. This is reflected by the persistent nystagmus and explains the dizziness when a patient is tilted backward.
Canalithiasis theory
In 1980, Epley published his theories regarding canalithiasis. [3] He thought that the symptoms of BPPV were much more consistent with free-moving densities (canaliths) in the posterior SCC rather than fixed densities attached to the cupula. While the head is upright, the particles sit in the PSC at the most gravity-dependent position. When the head is tilted back supine, the particles are rotated up approximately 90° along the arc of the PSC. After a momentary (inertial) lag, gravity pulls the particles down the arc. This causes the endolymph to flow away from the ampulla and causes the cupula to be deflected. The cupular deflection produces nystagmus. Reversal of the rotation (sitting back up) causes reversal of the cupular deflection and thus dizziness with nystagmus beating in the opposite direction.
This model can be compared with pebbles inside a tire. As the tire is rolled, the pebbles are picked up momentarily and then tumble down with gravity. This tumbling triggers the nerve inappropriately and causes dizziness. Reversal of the rotation obviously causes reversal of the flow and reversal of the dizziness direction.
Canal densities would better explain the delay (latency), transient nystagmus, and reversal on return to upright than would cupular densities. This supports canalithiasis rather than cupulolithiasis as the mechanism for classic BPPV.
The canalithiasis theory received further corroboration by Parnes and McClure in 1991 with the discovery of free densities in PSC at surgery.
Epidemiology
Frequency
United States
In one study, the age- and sex-adjusted prevalence of BPPV was 64 per 100,000. Other studies corroborate this finding.
Race
Little published information is available on racial predilection.
Sex
The sex distribution seems to indicate a predilection for women (64%).
Age
BPPV seems to have a predilection for the older population (average age, 51-57.2 y). It is rarely observed in individuals younger than 35 years without a history of antecedent head trauma.
-
The patient is placed in a sitting position with the head turned 45° towards the affected side and then reclined past the supine position.
-
The patient is then brought back up to the sitting position.
-
Next, the patient is rolled 180° from the affected side to the opposite side. Note that the position of the head is 45° toward the affected side before the roll. The head winds up facing down, 180° away from the starting position.

