Background
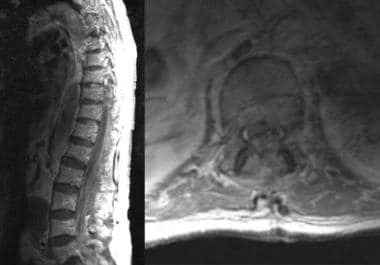
Epidural hematoma (ie, accumulation of blood in the potential space between dura and bone) may be intracranial (EDH) or spinal (SEDH) (see the image below). Intracranial epidural hematoma occurs in approximately 2% of patients with head injuries and 5–15% of patients with fatal head injuries. Intracranial epidural hematoma is considered to be the most serious complication of head injury, requiring immediate diagnosis and surgical intervention. Intracranial epidural hematoma may be acute (58%), subacute (31%), or chronic (11%). Spinal epidural hematoma may also be traumatic, though it may occur spontaneously. [1]
Etiology
Most epidural hematomas result from arterial bleeding, typically due to a tear of the middle meningeal artery or one of its branches when a temporal bone fracture crosses the pterion. Brisk arterial flow then strips the dura from the inner table of the skull, forming a rapidly expanding epidural collection. [2]
Less common traumatic mechanisms include injury to dural venous sinuses or diploic veins in the setting of minor skull fractures.
Spontaneous or iatrogenic causes are rare and include:
-
Coagulopathy or anticoagulation (eg, warfarin, direct oral anticoagulants, thrombolysis)
-
Invasive spinal procedures (lumbar puncture, epidural anesthesia)
-
Neoplastic involvement of the dura (metastases, leukemia)
-
Dural or skull-based vascular malformations
-
Paget disease of bone with cortical remodeling
Pathophysiology
Cranial epidural hematoma
Epidural hematoma usually results from a brief linear contact force to the calvaria that causes separation of the periosteal dura from bone and disruption of interposed vessels due to shearing stress. Skull fractures occur in 85–95% of adult cases, but they are much less common in children because of the plasticity of the immature calvaria. Arterial or venous structures may be compromised, causing rapid expansion of the hematoma; however, chronic or delayed manifestations may occur when venous sources are involved. Extension of the hematoma usually is limited by suture lines owing to the tight attachment of the dura at these locations. Recent analyses have revealed that epidural hematomas may actually traverse suture lines in a minority of cases. [3]
The temporoparietal region and the middle meningeal artery are involved most commonly (66%), although the anterior ethmoidal artery may be involved in frontal injuries, the transverse or sigmoid sinus in occipital injuries, and the superior sagittal sinus in trauma to the vertex. Bilateral epidural hematomas account for 2–10% of all acute epidural hematomas in adults but are exceedingly rare in children. Posterior fossa epidural hematomas represent 5% of all cases of epidural hematomas.
Spinal epidural hematoma
Spinal epidural hematoma may be spontaneous or may follow minor trauma, such as lumbar puncture or epidural anesthesia. Spontaneous spinal epidural hematoma may be associated with anticoagulation, thrombolysis, blood dyscrasias, coagulopathies, thrombocytopenia, neoplasms, or vascular malformations. The peridural venous plexus usually is involved, though arterial sources of hemorrhage also occur. The dorsal aspect of the thoracic or lumbar region is involved most commonly, with expansion limited to a few vertebral levels.
Epidemiology
Prevalence
Epidural hematoma occurs in about 10% of moderate to severe traumatic brain injuries and in about 1% of mild injuries. It is most common in adolescents and young adults, especially those aged 20 to 30 years. Motor vehicle collisions, falls, and assaults account for the majority of cases. [4, 5] Traumatic epidural hematoma has an overall incidence of 8.2% and requires surgery in 55.5% of cases, amounting to approximately 3.1 million operations worldwide each year. [6]
Intracranial and spinal epidural hematomas are more frequent in men, with a male-to-female ratio of 4:1.
Intracranial epidural hematoma is rare in individuals younger than 2 years. It is also rare in individuals older than 60 years because the dura is tightly adherent to the calvaria.
Spinal epidural hematoma has a bimodal distribution with peaks during childhood and during the fifth and sixth decades of life. Increasing age has been noted as a risk factor for postoperative spinal epidural hematoma.
Mortality/Morbidity
The mortality rate associated with epidural hematoma has been estimated to be 5–50%.
The level of consciousness prior to surgery has been correlated with mortality rate: 0% for awake patients, 9% for obtunded patients, and 20% for comatose patients.
Bilateral intracranial epidural hematoma has a mortality rate of 15–20%.
Posterior fossa epidural hematoma has a mortality rate of 26%.
Prognosis
The prognosis of an epidural hematoma is determined primarily by patient age, level of consciousness on presentation, associated intracranial injuries, and time to surgical evacuation. Mortality rises with advancing age and comorbid brain injury. Patients who are awake (Glasgow Coma Scale 13–15) at presentation have essentially 0% mortality, whereas comatose patients (GCS ≤ 8) face up to 40% mortality. Delay in evacuation beyond the so-called golden window (generally 4–6 hours from injury) is associated with a marked increase in both morbidity and mortality. In spinal epidural hematomas, the presence of T2‐weighted intramedullary hyperintensity on MRI predicts poorer neurological recovery. [7]
-
This MRI demonstrates spinal epidural hematoma.
-
CT scanning performed before and after surgical evacuation of an intracranial epidural hematoma.