Practice Essentials
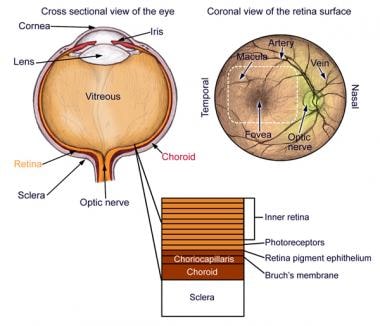
Uveitis is defined as inflammation of the uveal tract, which is further subdivided into anterior and posterior components. The anterior tract is composed of the iris and ciliary body, whereas the posterior tract includes choroid. Hence, uveitis is inflammation of any of these components and also may include other surrounding tissues such as sclera, retina, and optic nerve. [1] Uveitis often is idiopathic but may be triggered by genetic, traumatic, immune, or infectious mechanisms.
Signs and symptoms
Symptoms of uveitis depend on several variables, the most important of which are type (ie, anterior, posterior, intermediate) and duration of symptoms (ie, acute, chronic). Furthermore, a thorough review of systems (eg, shortness of breath, arthritis, rash, trauma, back pain, travel history, etc) should be conducted to elucidate potential underlying etiologies.
Acute anterior uveitis presents as follows:
-
Pain, generally developing over a few hours or days except in cases of trauma
-
Redness
-
Photophobia
-
Blurred vision
-
Increased lacrimation
Chronic anterior uveitis presents primarily as blurred vision and mild redness. Patients have little pain or photophobia except when having an acute episode.
Posterior uveitis presents as follows [2] :
-
Blurred vision and floaters
-
Absence of symptoms of anterior uveitis (ie, pain, redness, and photophobia)
The presence of symptoms of
Background
Uveitis is defined as inflammation of the uveal tract, the anatomy of which includes the iris, ciliary body, and choroid.
The iris regulates the amount of light that enters the eye, the ciliary body produces aqueous humor and supports the lens, and the choroid provides oxygen and nourishment for the retina.
A classification scheme for uveitis exists based upon anatomic location. [7]
Table 1. Classification of Uveitis (Open Table in a new window)
Type |
Primary Site of Inflammation |
Manifestation |
Anterior uveitis |
Anterior chamber |
Iritis/iridocyclitis/anterior cyclitis |
Intermediate uveitis |
Vitreous |
Vitreitis/hyalitis/pars planitis |
Posterior uveitis |
Choroid |
Choroiditis/chorioretinitis/retinochoroiditis/retinitis/neuroretinitis |
Panuveitis |
Anterior chamber, vitreous, and/or choroid |
All of the above |
Uveitis, particularly posterior uveitis, is a common cause of preventable blindness, so it is deemed a sight-threatening condition. Anterior uveitis is the form most likely to present to the emergency department. When the inflammation is limited to the iris, it is termed iritis. If the ciliary body is also involved, it is called iridocyclitis.
After anatomic classification, uveitis is further described by the following [8] :
-
Onset (sudden vs insidious)
-
Duration (limited, < 3 months in duration; persistent, >3 months in duration)
-
Course (acute, recurrent, or chronic)
-
Laterality (unilateral vs bilateral)
The distribution of general uveitis cases by anatomic site of disease has been found to differ significantly between community-based practice (anterior, 90.6%; intermediate, 1.4%; posterior 4.7%; panuveitis, 1.4%) and university referral practice (anterior, 60.6%; intermediate, 12.2%; posterior, 14.6%; panuveitis, 9.4%; P< 0.00005). [9]
Pathophysiology
The etiology of uveitis varies between populations and often is idiopathic [8] ; however, genetic, traumatic, or infectious mechanisms are known to promote or trigger uveitis. Diseases that predispose a patient to uveitis and are likely to present to the emergency department include inflammatory bowel disease, rheumatoid arthritis, systemic lupus erythematosus (SLE), sarcoidosis, tuberculosis, syphilis, and AIDS.
The mechanism for trauma is believed to be a combination of microbial contamination and accumulation of necrotic products at the site of injury, stimulating the body to mount an inflammatory response in the anterior segment of the eye. [8, 10]
For infectious etiologies of uveitis, it is postulated that the immune reaction directed against foreign molecules or antigens may injure the uveal tract vessels and cells.
When uveitis is found in association with autoimmune disorders, the mechanism may be a hypersensitivity reaction involving immune complex deposition within the uveal tract.
In one study at a tertiary referral center by Rodriguez et al, [11] the distribution in etiology among all anatomic forms of uveitis, anterior, intermediate, and posterior, were as follows:
-
Idiopathic (34%)
-
Seronegative spondyloarthropathies (10.4%)
-
Sarcoidosis (9.6%)
-
Juvenile rheumatoid arthritis (JRA) (5.6%)
-
SLE (4.8%)
-
Behçet disease (2.5%)
-
AIDS (2.4%)
Seronegative arthropathies include nonspecific, ankylosing spondylitis, Reiter syndrome, psoriatic arthropathy, and inflammatory bowel disease.
In the same Rodriguez et al study, [11] anterior uveitis was the most common form at 51.6%, and the etiologic distribution was as follows:
-
Idiopathic (37.8%)
-
Seronegative arthropathies (21.6%)
-
JRA (10.8%)
-
Herpes virus (9.7%)
-
Sarcoidosis (5.8%)
-
SLE (3.3%)
-
Rheumatoid arthritis (0.9%)
Posterior uveitis was next most common, with 19.4% of cases, the most common etiologies being Toxoplasma (24.6%), idiopathic (13.3%), cytomegalovirus (CMV) (11.6%), SLE (7.9%), and sarcoidosis (7.5%).
A more rare cause of uveitis are medications. Few studies and case reports have associated bisphosphonates, fluoroquinolones, hormone replacement therapy, and etanercept with the development of uveitis. [12]
Frequency
United States
The approximate estimated annual incidence of uveitis in the United States ranges from 25-52 cases per 100,000 persons per year. [4, 13, 14] A 2021 systemic review found the estimated prevalence of non-infectious uveitis to be 121 per 100,000. [12]
International
The incidence and prevalence of uveitis vary widely internationally. Finland has one of the highest annual incidences of uveitis, probably because of the high frequency of HLA-B27 spondyloarthropathy among the population. [4] The reported prevalence of uveitis (infectious and non-infectious) in China ranged from 152 per 100,000 in China; 173 per 100,000 in South Korea; 194 per 100,000 persons in Taiwan; and 317-730 per 100,000 in India. [12]
Race
Racial predisposition to uveitis is related to the patient's underlying systemic disease, as follows [2] :
-
Whites: HLA-B27, multiple sclerosis
-
Blacks: Sarcoidosis, SLE
-
Mediterranean/Middle Eastern descent: Behçet disease
-
Asians: Behçet disease
Sex
In general, uveitis has no sexual predisposition except in cases secondary to autoimmune diseases, which are more common in women compared to men. [2, 12]
Age
Most people who develop uveitis are aged 20 to 50 years.
Mortality/Morbidity
No deaths due to iritis or uveitis have been reported.
Uveitis has been reported to be responsible for 5-20% of total blindness in Europe and North America and up to 25% of blindness in the developing world. [15, 12]
Morbidity results from posterior synechiae formation (adhesions between the iris and the lens) that may lead to high intraocular pressure, optic nerve loss and visual impairments. Blindness may result from inadequate treatment. Complications of medications, specifically topical steroids, may include glaucoma, cataracts, and potential vision deterioration. [1, 16]
Prognosis
Generally, the prognosis for iritis and uveitis is good with appropriate treatment. However, uveitis can be recurrent and affect the contralateral eye, especially with underlying inflammatory diseases.
-
Anatomy of the eye.
-
Small stellate keratic precipitates with fine filaments in a patient with Fuchs heterochromic iridocyclitis.